health care
CONCEPTUAL GUIDE TO THE HEALTH CARE MODULE
Prepared by Pat Armstrong, Katherine Laxer and Hugh Armstrong
INTRODUCTION
Categories, and their definitions, matter. All social data are gathered based on a particular framing of questions. These questions themselves reflect a specific way of seeing and understanding social factors, forces, processes and relations. The answers to questions are then grouped into categories based on concepts of both what is important and how aspects relate to each other. As Deborah Stone, the noted American feminist puts it, no number is innocent (Stone 1988: 130). The purpose of this conceptual guide is to suggest questions that need to be asked before the data in this module are used and to provide some analysis of the data available to develop a picture of work in the health care industry.
Because concepts matter in the production and configuration of social data, the conceptual guide to the Health Care Module explores the concepts at work in Statistics Canada data on the health care industry. It begins by looking at how health care is defined, because the understanding of care shapes the data on who is included or excluded as workers in care. The concepts behind the data, we argue, indicate ways of seeing health care work that are integrally related to the undervaluing of women’s work and that ignore critical perspectives on health. These concepts in turn are linked with those defining public and private care in the formal economy, the community and the household. Like other categories, those on the structure of work and workplaces reflect simultaneously actual changes in the work organization and conceptualizations of those changes. Similarly, the categories used for the collective organization of care providers into unions and professions both indicate how people resist and ideas about differences in forms of resistance. Finally, our conceptual guide turns to the data on the health of health care workers, arguing that while the data records alarming rates of illness and injury, the gendered nature of the work and of the definitions for workplace hazards are largely ignored.
KEY CONCEPTS
Women, health and care
A gendered analysis of health care work requires an understanding of what is meant by health and care. How we conceptualize the distinctions has profound implications for what is included in our analysis, as well as how we approach the analysis. In 1947, the World Health Organization (WHO) defined health as “a state of complete physical, mental, and social wellbeing and not merely the absence of disease and infirmity” (WHO 1986). This definition grew out of and contributed to what has come to be known as a determinants of health approach. It was reflected in Canada by the Lalonde Report, a seminal document produced by the then federal Minister of Health and Welfare (Canada 1974).
From this perspective, health is also socially constructed rather than simply biologically determined or technically produced. According to the 1986 Ottawa Charter, a product of the First International Conference on Health Promotion, “Health is created where people live, love, work and play”. The Ottawa Charter defined health promotion as “the process of enabling people to increase control over and to improve their health” (Canada 1986). Creating health means building healthy public policy; creating supportive work, home and community environments; strengthening community action; developing personal skills; and reorienting health services to be health promoting rather than simply treatment focused. The subsequent Adelaide Conference in 1988 defined health as a fundamental human right and stressed the importance of equity, identifying improvement of women’s health as a priority not only because women suffer from inequality but also because they are critical in the daily promotion of health. Three years later, the Sundsvall Conference in 1991 highlighted the spiritual, social, cultural, economic, political and ideological dimensions of environments. In other words, a determinants of health approach tells us that health is critically influenced by social and physical environments, by relations as well as by structures or technologies, and not only by genes.
Health is thus created everywhere, not only within the formal health care system. And it is created in classed, racialized and gendered ways. Feminists throughout the world have emphasized the centrality of gender in the creation of health, and the gendered consequences of subordinate relations and conditions. These relations, relations that are critical in determining health are relations of ruling, as Clement and Myles (1994) put it, with women participating on unequal terms with men. The Fourth World Conference on Women (the Beijing Conference 1995) agreed that “Women’s health involves women’s emotional, social, cultural, spiritual and physical well-being and is determined by the social, political and economic contexts of women’s lives as well as by biology”. These conclusions were based on and contributed to a broad literature establishing the invisibility and under-valuing of women’s health and women’s health care work. Equally important in this literature is the question of differences among women, differences related to their various social, cultural, physical and economic locations as well as to their abilities.
Canadians have been active participants in the construction of the social determinants of health approach (e.g. Raphael 2009; Raphael, Bryant and Rioux 2006), and in the demand for a gender-sensitive analysis and strategy in health. Health Canada recognizes 12 distinct determinants of health, although the list has changed over time (Robertson 2001). Indeed, any such listing is necessarily arbitrary, informed by ideology as well as by evidence. Moreover, the elements overlap and interact with each other in ways that challenge any notion of firm divisions. Like biology and gender, the other ten health determinants are changeable, albeit in the context of what is inherited in a particular society. The determinants are all about political choice and about material conditions, about both the collective and the individual. And they are all about gender. The 12 are worthwhile considering precisely because they reflect all these aspects of policy and the social construction of data.
1. Biological and Genetic Endowments. Women’s bodies are different from those of men, and thus so too are their health issues. However, there is an enormous variation among women and not everyone can be easily sorted into a male or female biological category. The acknowledgement of sex differences often means a focus on reproductive health (breasts and babies), but the range of issues is much broader (e.g., indications of heart attack, processing of pharmaceuticals, responses to work environments). Biology is often seen as unchangeable, but in fact it is influenced by social contexts, contexts that are unequally structured for women and men as well as for different groups of women (e.g., lowered average puberty age and increased average height with improved living standard, class differences in birth processes). Even genes can be influenced by the environment and their meaning is influenced by the environment.
2. Gender. This term is of course used to draw particular attention to the social construction of female/male differences. Gender is an important feature of how individuals experience a world characterized by systematic patterns of oppression, with widespread inequality along structural, social and ideological dimensions. One expression of this is unequal opportunities by gender for health and health care. One result is the development of gender-based analysis, a tool for understanding, and improving how public policy is made. Such an approach does much more than analyze data by sex; it takes into account the contexts and relations in women’s lives. Thus, another is the adoption of research strategies that begin with the daily activities that shape the lives of women and men. In addition to being a specific determinant, gender pervades all the other determinants.
3. Income and Social Status. It should be noted that this Health Canada category is not titled Class and Power, reflecting a particular view of material inequality. Nor does it address issues of wealth. It nevertheless recognizes some inequality linked to money and to ideas about worth. Research has established that industrial societies with the narrowest income disparities (e.g., Japan, Sweden) have the best health outcomes while those with the widest disparities (e.g., US, UK) have the worst outcomes (Wilkinson 1992; Wilkinson and Pickett 2010). In other words, the greater the inequality in a society, the poorer the health of its population, whether rich or poor. Moreover, within a society, there is a positive statistical relationship between higher incomes and better health, throughout all income levels. The richer you are, the better your chances of enjoying good health. Women have less income than men from wages and salaries and from property, and they suffer from more health problems than men. For example, in 2009, more than half of the women in the lowest twenty percent income bracket have two or more chronic health conditions (Statistics Canada 2012a: 9). Lone parent mothers are particularly likely to be poor. The absence of a universal child care program for pre-school children in all but Quebec makes it very difficult for such women to participate in the paid labour force. Meanwhile, reductions in state welfare support severely limit women’s income when they do stay home to care for the children. Sharp reductions in the number of people cared for in hospitals or other institutions further adds to women’s workload especially, often making it difficult to participate full time in the labour force.
4. Employment. Unemployment is bad for one’s health. Although their official unemployment rate has in recent years been slightly lower than that of men, women are more likely to be discouraged from actively seeking paid work, both because they have family responsibilities and because they face discrimination in the labour force. These factors, combined with the fact that unemployment data only count those actively seeking work now, mean that the number of women who want and need paid work is particularly under-estimated. Underemployment and precarious employment can also be bad for one’s health. Women are much more likely than men to be working part-time and part-year while seeking full-time, full-year work, and thus to be in effect partially unemployed (Vosko, MacDonald and Campbell 2009). Women are also more likely to be what Statistics Canada calls own-account self-employed. As Vosko and Zukevich (2003) point out, such work is often just another form of part-time, precarious employment. Indeed, even when women have full-time, full-year paid work, their employment conditions and pay often make the work precarious (See the precarious employment module). And because almost all women have a second job at home doing the domestic and caring work they face the unhealthy stress of managing two jobs. In the labour force as at home, women perform different jobs than do men. Sex segregation in paid work means that women are more likely to be in low status/high stress jobs, jobs that undermine health (Armstrong 1996; Armstrong, Armstrong and Scott-Dixon 2008). However, their health hazards usually go unrecognized because it is women’s work (Messing 1998; Vogel, 2003; Le Jeune, Belisle and Messing 2008).
5. Education. The more education a person has, the better their health is likely to be. Following long struggles for equal opportunity, Canadian women are now more likely than men to have completed secondary school and college, and are as likely to be enrolled in undergraduate university degree programs. Many more have moved into medicine and pharmacy as a result of barriers coming down in university entrance practices. Women tend to be enrolled in different programs, however, leading to different jobs and pay levels. Because women still bear the primary responsibility for children, educating women has a large impact on the education of children and thus on their health.
6. Physical Environments. Physical environments include traditional public health concerns such as clean air and water, pure food and drugs, housing and aggressive actions against infectious disease. They also include such factors as gun control and street safety, transportation (especially public mass transit which is used disproportionately by women and children) and access to natural light in workplaces. Household hazards such as cleaning materials and chemicals are also an issue for women in particular, since women do more domestic work and spend more time at home than men (Rosenberg 1990). Equipment and light, space and time are all part of the physical environment which, like the rest, affect, and are affected by, gender differentially.
7. Social Environments. Environments are not only about physical structures. They are also about social relations. Most women are less powerful than most men and therefore less able to resist sexual harassment and violence. Power also varies with racialized groups and immigration status. Men are more often involved in violence, however, and frequently suffer physically as a result. Values too are part of the environment that influences health. Both women and their work are often undervalued compared to men. Moreover, dominant attitudes can also undermine health. Welfare policies, for example, reveal the gendered ways in which society is organized. Reductions in assistance rates affect women in particular, because they are the majority of those on welfare, and the reductions do more than lower income; they also send a message about worth.
8. Social Support Networks. Social support is critical to health, and women are more likely to give and receive such support than men. Women are more likely to foster social contacts, which are healthy. However, they are also more likely than men to live alone as they get older, because they tend to marry older men, and also to live longer. Compared to previous generations, women have fewer children, and frequently see those few children leave home and move to other communities, often hundreds or thousands of kilometres away.
9. Healthy Child Development. This health determinant cannot be separated from conditions for healthy mothers, although it is often presented as if this were the case. Ages 0-5 are now viewed as particularly important for mental and physical growth, but social supports for childrearing, such as child care services and welfare payments, have been reduced in recent years at the same time as the pressure on women to work for pay has increased. Yet mothers are still held primarily responsible for child development and are too often blamed when things go wrong.
10. Personal Health Practices and Coping Skills. While the previous health determinants are at least as much social and collective as they are individual and personal, this determinant is primarily defined as being about our own habits and the initiatives taken to maintain, improve or risk our health. Yet mothers are often held responsible, blamed for their partner’s and children’s nutrition, personal hygiene and health education. Moreover, the interpretation of this determinant usually ignores the role social structures play in creating our possibilities for healthy life styles and behaviours. Moreover, the time involved in practicing a healthy lifestyle is seldom discussed, ignoring the poverty experienced by many women.
11. Culture. The term culture is used, but it could be interpreted to encompass the health hazards of racialization as well. As is the case with income and social status, the terms used imply a particular way of viewing social relations. Canada is described as a multicultural society, with annual immigration exceeding 200,000, from all corners of the world. Immigrants frequently experience a decline in health status after they come to Canada. There are multiple reasons for this decline, including immigrant women’s more limited access to training in one of the two official languages which restricts their ability to participate fully in Canadian society. Meanwhile, the Aboriginal peoples who make up about 6% of the population have appreciably lower health status than the rest of Canadians, including immigrants. There are some strategies underway to combat racism, to curb the global transfer of diseases, and to ensure equitable access to health education and health care, but there is still a long way to go.
12. Health Services. Health services are defined as only one of the determinants of health. Health services are a women’s issue (Armstrong et al. 2002; Grant et al. 2004, 2012; Armstrong and Armstrong 2010) for the following reasons. Women are the overwhelming majority of those providing care. They are also a majority of those receiving health care, although they are a minority of the formal decision-makers in health services. Thus, changes in care such as increased financial or other barriers particularly affect women, especially given their lower incomes. Differential treatment issues are just beginning to enter public media and health care practices themselves. For example, there is evidence of more diagnosis of heart attacks in men and of symptoms as solely psychological for women, resulting in more prescribing of mood-altering drugs for women and surgery for men. These determinants reflect a shift in thinking from an exclusive emphasis on curative to health promotion approaches, at least in theory and policy discourses.
In spite of the emphasis on the social, however, this list of determinants largely ignores the larger issue of political economies and power inequalities at the global, national and local levels and the ways political economies influence health and care. The most popular determinants of health approaches provide no context for the social determinants of health (Poland et al., 1998). And there is little explanation for changes over time or among groups, except for those explanations that look to individual practices or values. “Globalization” is usually seen as primarily a matter of international trade in goods, services and to a lesser extent people. Yet the international, unequal movement of capital, of information, of culture and of workers sets the stage for each of these determinants. International agreements are negotiated and enforced mainly through the World Trade Organization (WTO). The most obviously relevant for health are TRIPS (Trade Related Aspects of International Property Rights), important for drug patents and patenting life forms, GATS (General Agreement on Trade in Services) and CETA (The Canada-European Union Comprehensive Economic & Trade Agreement), significant in terms of drug costs and ownership of services, given that in the industrialized world such services account for two-thirds of all jobs. Whether Canadian health care is subject to these agreements is a matter of debate, although the 2002 Romanow Commission on the Future of Health Care (Canada 2002: chap.11) warned that the public system of care is at risk and urged clarification to protect public care. We are still waiting. The rules for health care workers are even less clear. However, there is no question that there is a large international market in female-dominated occupations such as nursing and that global agreements influence health and care (Bourgeault et al. 2010).
The implications for health care work
In the Health Canada list of determinants, health care is one of twelve influences on health. Yet most of the other eleven have a profound impact within health care. Indeed, their impact may be even greater within care. So, for example, while social and physical environments are important to everyone, those who are ill have compromised immune systems that make them particularly vulnerable to germs found in bathrooms and are especially in need of social support. Similarly, culturally unresponsive environments may be even more threatening for those who are ill and feeling vulnerable. And while secure employment is important to all those who need paid work, in the case the health care workers precarious employment could translate into poor care that has significant health consequences for those needing services.
Beginning with the social determinants of health, then, has implications for the study of health care work (Armstrong, Armstrong and Scott-Dixon 2008). It means that all those employed in the health sector are recognized as contributing to health, whether they assist in surgery or clean up after surgery, whether they administer drugs or feed patients, whether they determine the prescriptions or keep records of them. This may seem obvious, and it certainly was to Florence Nightingale who began her crusade to improve care by cleaning up the hospitals. Those federal politicians who approved the Canada Health Act, the legislation that sets out the principles for Canada’s public system, also recognized that hospital care involves the full range of occupations employed in that institution. Indeed, the Act specifically includes everyone who works in the hospital.
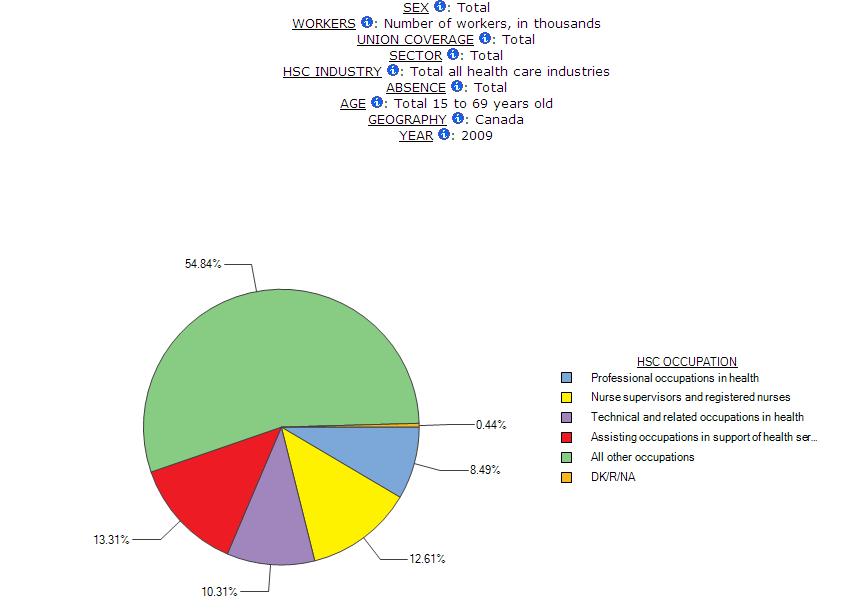
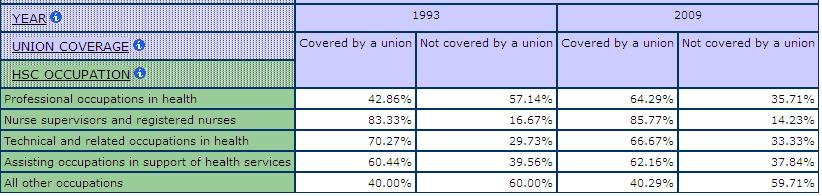
However, many studies of health care providers focus on occupations more obviously directly linked to treatment and cure. For example, the Canadian Institute for Health Information produces reports on health care providers that look mainly at nurses and doctors, although some other professionals such as pharmacists and technicians are also included (CIHI 2013). There is no mention of those who cook and clean or who do laundry, clerical and maintenance work or any of the other jobs often defined as ancillary or support work (Armstrong, Armstrong and Scott-Dixon 2008). The Statistics Canada industry category of healthcare should include such a wide range of providers. Statistics Canada[i] explains that industry data are constructed within a supply-based, or production-oriented, conceptual framework where establishments using similar production processes to produce goods and services are grouped to form industries. The boundaries between industries demarcate, in principal, differences in production processes and production technologies. This would suggest that everyone who works in health care would be included in the Statistics Canada health care category in ways that recognize the determinants of health. And many of them are. According to the 2009 Survey of Labour and Income Dynamics (SLID), 54.8% of those employed in the health care industry are in what are sometimes called ancillary services or support work (Chart 1 – “all other occupations”). Less than half of the paid workers counted as part of the health care industry by Statistics Canada are defined as “health care occupations” – or sometimes called direct workers. Chart 1 depicts the occupational composition of the entire health care industry in Canada in 2009 using SLID data. Our multidimensional tables in the Health Care Module use this categorization of occupations so that users can compare what are typically classified at “health occupations” including professional occupations in health, nurse supervisors and registered nurses, technical and related occupations in health, assisting occupations in support of health services with the category of “all other occupations”. This last category includes clerical workers, cleaners, maintenance workers, security guards, laundry staff, food service workers, among others.
Chart 1 – Occupational Composition of the Health Care and Social Assistance Industry, Canada, SLID 2009
In spite of the large share of ancillary occupations within the health care industry, these data increasingly leave out many of these ancillary workers narrowing the estimate presented here. Ancillary occupations are misclassified for two linked reasons (Armstrong, Armstrong and Scott-Dixon 2008). First, the struggle for recognition of both skills and contribution to health continues for those who have taken on the tasks previously done mainly by nurses and traditionally by women. More of the work is not only being defined out of care but also contracted out to firms that have no experience in health care delivery. For example, the 2002 Romanow Report on the Future of Health Care in Canada drew a line between the jobs defined as direct and those defined as ancillary, implying that ancillary services are not really about health care. Although the Romanow Report did not offer a specific definition of ancillary services, it did describe them as services “such as food preparation, cleaning and maintenance” (Canada 2002: 6). Clerical, security and laundry workers would also seem to fit in with this understanding of ancillary, given that these workers too do not provide “direct” care. Although the Report suggested that ancillary services could be safely separated from the public sector and contracted to for-profit concerns, it contains no evidence to support this form of privatization. Such a separation assumes that these workers are not critically involved in health care delivery. Some provinces have made this assumption. They have redefined the work as “hotel services” and much of it has been contracted out.
Second, when ancillary services are contracted out, Statistics Canada, using the North American Industrial Classification System (NAICS), can classify them under an industry other than health. For example, contracted food services are likely to fall within the accommodation and food services industry rather than health care even though these services may be engaged to prepare and serve food in a hospital. Although workers in these contracted out services may continue to work in a health care service, their employer may no longer be the health care facility but some other establishment in another industry. Hence, the NAICS presents an important challenge for profiling ancillary occupations in the health industry. In sum, when the claim is made that “Professionals made up 57% of all workers in the health sector in 2001” (Galarneau 2004: 14), it is important to ask who was included in the health sector, and what difference it would make if all the cooks, cleaners, clerks, and laundry, maintenance and security workers were counted.
It should also be remembered that labour force data capture only those who said they worked for pay. Yet much of the care work is done by volunteers and family members who provide this care both in and outside care facilities (Grant et al. 2004; Armstrong 2013a) with implications for their participation in paid work (Lilly, Laporte and Coyte 2010) and their participation in social life (Yantzi, Rosenberg and McKeever 2007). According to Statistics Canada, approximately 3 billion hours of voluntary health care work is done each year, significantly more than the number of paid hours. However, volunteers cover a very broad range of activities, including information exchange, public awareness, education, support, fundraising, advocacy, public dialogue and policy development, as well as direct care. In other words, many of these volunteers are involved in broadly defined determinants of health rather than in direct care. Care hours provided by family members are hard to calculate with any precision. As a result, data based on paid work provides only part of the picture. Indeed, it may provide only the smaller part, because research suggests that the majority of care – 85% to 90% – is provided by people not paid for the job (Denton 1997).
This module is based on the health care industry. Like all categories, this one does not simply reflect facts; it also reflects assumptions. Industrial categories are supposed to be based on where people work. Such an approach could accommodate the determinants of health research because it would capture the full range of services provided in facilities. But health reform strategies, Statistics Canada methods for organizing data, along with databases housed at the Canadian Institute for Health Information, leave out many of the workers that a determinants of health approach suggests should be included. And both the old and the new means of constructing industrial categories leave out the many people who provide unpaid care. Given what we know about who provides care, we can assume that most of those left out are women.
INDICATORS
Several indicators used within the Health Care Module overlap with and are described by other modules of the GWD. These include indicators of social location (e.g. sex, immigrant status, visible minority status, age), indicators of precarious employment (e.g. firm size, hourly wages, union coverage), and indicators of the employment relationship (e.g. temporary, permanent, part-time, full-time, class of worker). Indicators selected to reflect specific aspects of work in health care include indicators for care context (year, geography, sector), care providers (occupations including “all other occupations” which refers to workers in support provider occupations such as cleaning, food services, clerical or anything not classified within the Statistics Canada/NOCS category of “health occupations”), and health and well-being (work schedules, health status, absences).
DATA SOURCES
To build the statistical database for the Health Care Module, we use the Canadian Census (2001 & 2006), the Statistics Canada Survey of Labour and Income Dynamics (1993-2009), and the Statistics Canada Labour Force Survey (1997-2008). In total, 26 multidimensional tables (15 new as of 2013, 11 updated from the original series) have been designed using these sources and users can tailor the layout of these tables to explore many aspects of health and social care work in Canada.
DEMONSTRATION 1
Health care is women’s work
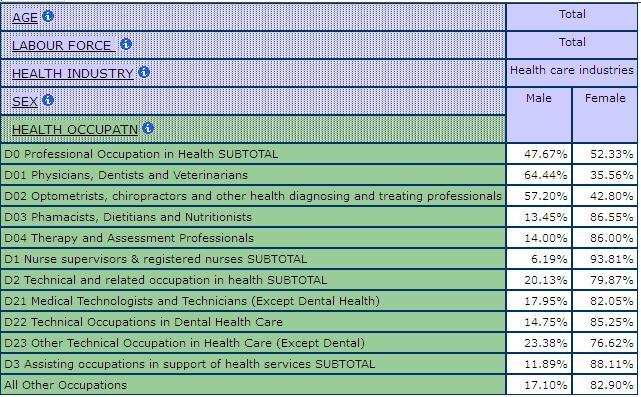
Regardless of how it is calculated, health care is women’s work. Four out of five paid workers in health care are women. Nurses constitute the single largest occupational category in health care, accounting for over 30% of those Statistics Canada counts as part of the health sector, and over 60% of health professionals. Meanwhile, according to 2006 Census data, 93.8% of nurses are women (Table 1). Until the discriminatory admissions policies for medical school began to be removed in the 1960s, the overwhelming majority of doctors were men. Women are still a minority of practicing doctors. In 2006, 35.5% of physicians, dentists and veterinarians were women. But women accounted for almost three quarters of the increase in the total physician workforce and almost all of the increase among GPs (Galarneau 2004). Women have made even faster progress in some other medical professional categories. For example, according to 2006 Census data, they made up 86.5% of pharmacists, dietitians and nutritionists (Table 1). It is interesting to note, however, that women have become pharmacists just as pharmacy has changed from an occupation that was made up primarily of self-employed professionals to one where most are employees of large drugstore chains. Women also dominate most of the other technical occupations in the health care field. The overwhelming majority of technicians and therapists are women and their proportions are increasing in most of them. There are exceptions. Men are the majority of denturists, dental technologists, laboratory bench workers and of ambulance attendants. Overall, 79.8% of technical and related occupations in health care and social assistance are women (Table 1).
Statistics Canada includes some support personnel within the “health occupations” category. Among these workers classified as “assisting occupations in support of health services” women dominate. 88% are female (Table 1). This category includes dental assistants care aides, orderlies and personal assistants and concentrations of women are very high in all of these occupations. Indeed, these jobs are more female-dominated than the professional occupations in health. However, these other support personnel do not include all of those who cook, clean, do laundry and keep records. Ancillary occupations or “all other occupations” within the health and social assistance industry not classified as health occupations constitute over half of the paid workers in this more broadly defined sector, and, again, most of them are women. They cook and clean, undertake clerical work, and serve as either childcare or home support workers.
Table 1: Shares of Men and Women by Health Occupation, Canada, 2006 Census
There is a notion that support work in health care requires few skills, a notion that reflects both the female dominance of health care work and the traditional male dominance of medicine. It does not reflect the literature on the determinants of health or the feminist literature on skills (see, for example, Armstrong 2013b; Gaskell 1986). Medical men played a key role in the development of the Canadian health care system. Their model of practice stressed the intervention through surgery and drugs, or what is called allopathic medicine. In this model, doctors are scientists who base their treatment of body parts on the specialized knowledge of causes and cures. Their dominance is both justified and required in order to ensure effective diagnosis, treatment and cure (Armstrong and Armstrong 2003: ch. 2). These men and their model shaped the development of formal care systems. While women have continued to provide the majority of daily care, the doctors have long been in charge. Health care was and remains highly gendered and characterized by segregation in terms of occupations and by fundamental inequalities in power.
This medical dominance (Willis 1983) is reflected in the restructuring of formal health care services. Increasingly, only the most acute interventions are defined as requiring institutional care. Patients are sent home quicker and sicker at the same time as there is a move to day surgery and outpatient services. Clear lines are being drawn between acute and chronic care as well as between health services and other forms of care. Women have actively resisted this dominance at the same time as they have been complicit in its perpetuation. Initially, almost all of them were called nurses and few had formal training. Florence Nightingale and others helped change this, introducing training programmes and articulating the skills, as well as the duties, required of nurses. Through long struggle nursing became recognized as skilled. It also became more narrowly defined (Armstrong and Armstrong 2009).
As nurses gained recognition and power through their collective organizing, more and more of their work was carved off to be done by others. Here can be found the origins of the “ancillary” occupations. It was cheaper to hire others who could be more quickly trained and who had fewer formal qualifications. In part they could be quickly trained because as women they had already acquired many of the skills involved in the work. Moreover nurses sought to abandon many of these tasks as they increasingly defined themselves as professionals. The workers who inherited these tasks also struggled to have their skills recognized and their contributions valued in benefits and pay. They were less successful, however, in part because their skills were understood as common to women, making it much harder to argue their case. It seemed to many that the women who cook, clean and do laundry in health care are simply doing what any woman can do.
Yet there are skills involved in any such work and there are particular skills involved when the work is done in health care. The demands of this work are specific in health care. Health care cleaning staff, for example, must work around complicated, delicate equipment and living patients. Laundry workers in health care must carefully separate laundry, not in terms of colours and materials as we do at home, but rather in terms of diseases and patients. Laundry from isolation wards has to be washed in manually loaded machines and specially treated (Cohen 2001:12). Records must be meticulously kept in ways that require considerable specialized knowledge about health issues. Food preparation too requires such knowledge, with special care taken to ensure foods meets the specific dietary needs of the ill, frail and disabled.
The hazards are different in health care work. The risks of infection are greater and different in health care. The chemicals handled are dangerous and varied. Indeed, health care cleaners have three times the injury rate of other cleaners (Workers’ Compensation Board, quoted in Cohen 2001: 9). Health care laundry that has not been appropriately handled can become life-threatening for patients (Orr et al. 2002). It can also be dangerous to those doing the work, with hepatitis A or B providing only one example (Borg and Portelli 1999; Wa 1995). While food matters to us all, it is more critical in care. Food not eaten, the wrong food eaten or food eaten at the wrong time in the wrong way can be especially dangerous to the ill, frail or disabled. So can food that is not correctly prepared. Working around patients means not only exposure to disease but also to violence (Banerjee, Daly et al. 2008; Findorff et al. 2004; Morgan, Stewart, et al. 2005). Equipment not properly maintained can mean a life not saved. The environments for care are part of care, and can be as critical to health as clinical interventions. Indeed, they can influence whether such interventions succeed or fail. In addition, the consequences of mistakes or poor quality are more significant in health care than in other industries. A poor cafeteria meal may mean a hotel customer goes to another hotel but a poorly prepared meal in the hospital could mean the difference between recovery and continued illness. Of course, improperly stored or prepared food can harm people in either place. But ill people are more vulnerable. The wrong meal delivered to the wrong patient can have even more serious consequences. Invisible germs in hospitals can mean contagion and death for patients with weak immune systems. The wrong data recorded can cause life-threatening mistakes.
In short, there are skills involved in this work. The definition of the work as unskilled is as much a reflection of the gender and power relations in the work as it is of the nature of the jobs (Armstrong 2013c). This assumption has important consequences not only for those paid for the job but also for those who do the unpaid care. Pervasive contracting out of this work suggests that this is not a problem, indicating the failure to recognize either the skills involved in the work or their integral relationship to care. The result, as the next section demonstrates, is poorer conditions for those paid for the work.
Women not only constitute the primary paid workforce in health care. They also account for the overwhelming majority of those who provide the unpaid care in the home and as volunteers in the community (Duxbury, Higgins and Shroeder 2009; Duxbury and Higgins 2012; Grant 2004). When children or partners are sick, it is usually women who not only give medicine, take temperatures and clean catheters but who also do the extra or special cooking, cleaning and laundry. Women do this kind of work for neighbours and friends as well as for members of their extended families, whether or not they live in the same homes (Armstrong 2004). Statistics Canada has been a pioneer in counting such work (see, for example, Hall et al. 2001; Jones 2000; Luffman 2003; Zukewich 2003; Lindsay 2008) although the question on unpaid work in the now voluntary long form Census was removed in 2011. There are significant problems with the data that are available, particularly in terms of undercounting women’s work, as the section on social reproduction explains. However, the data that are available leave no doubt that most unpaid personal care is provided by women and so is most of the other work the social determinants of health literature indicates is about health care.
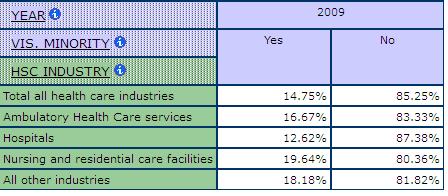
Which women
To say health care is women’s work does not tell us much about which women work in health care. Statistics Canada’s visible minority category does help us get some idea about access to jobs in health care and the distribution of jobs among women. Those women classified as visible minority account for approximately 12% of the employed, providing us with a comparator for work in the health industry. In general, the data suggest that visible minority women are slightly over-represented in direct health occupations and significantly overrepresented in some occupations within this category. The concentration of visible minorities also varies by sub-industry in health care and social assistance. For example, as shown in Table 2, among physicians and other professionals in ambulatory health care services, 31.2% are visible minorities, compared to 19.6% in hospitals. In nursing and residential care, there are higher concentrations of visible minorities working as nurse supervisors and registered nurses (21% compared to 13.2% in hospitals). The sub-industry in health care and social assistance with the highest relative concentration of visible minorities is nursing and residential care where 19.6% are visible minorities, compared to an average concentration of 14.7% across all industries in care (Table 3).
Table 2: Shares of Visible Minorities by Occupation and Sub-Industry, SLID 2009
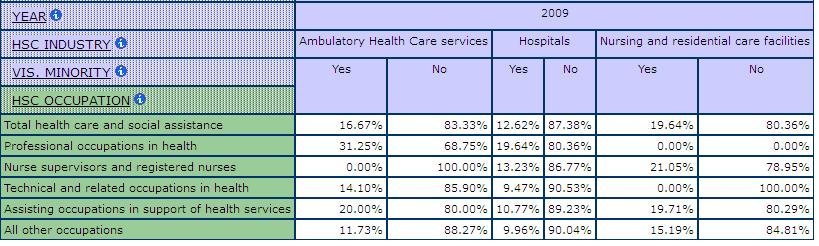
Table 3: Shares of Visible Minorities by Sub-Industry in Health Care and Social Assistance, SLID 2009
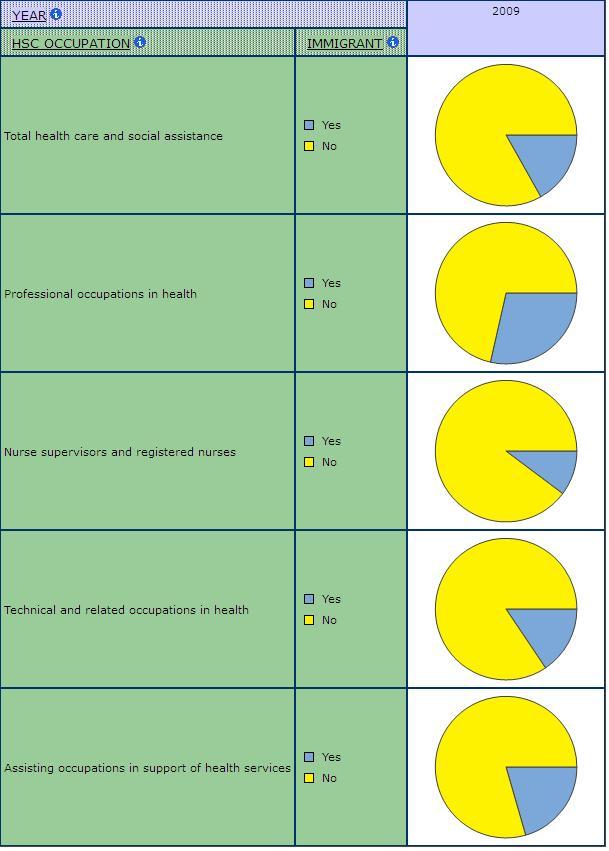
Immigrants are also overrepresented among some occupations and sub-industries in health care and social assistance. Chart 2 shows a visual depiction of the shares of immigrants and non-immigrants in the different occupations in care. Immigrants are overrepresented among physicians and other professionals and among the assisting occupations in support of health services (e.g. care aides, personal support workers).
Chart 2: Shares of Immigrants by Occupation in Health Care and Social Assistance, SLID 2009
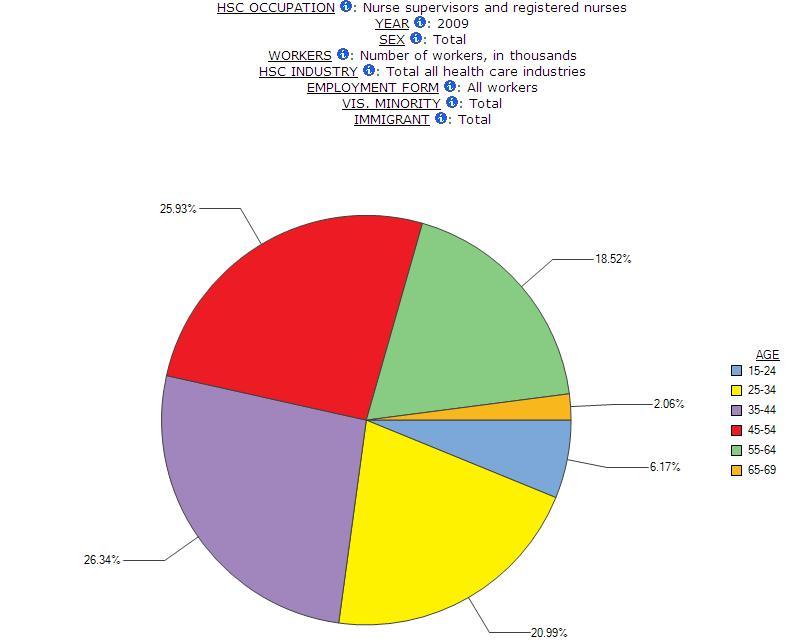
Any description of the health care labour force would be incomplete without reference to age. There was an influx of women into the labour force when the demand for health care workers began to grow significantly in the 1950s. Many have remained in, or returned to, their health care jobs. Table 4 shows a pattern of aging across all occupations in health care and social assistance. For example, between 1993 and 2009, the share of nurse supervisors and registered nurses between the ages of 55-64 grew from 12.8% to 18.5%. There has even been the emergence of a workforce of nurses past the typical retirement age of 65 over this time period (Chart 3 and Chart 4 show sample visualizations of this data that can be configured using the Beyond 20/20 tables in the Health Care Module). Across all occupations in health, the share of workers age 55-64 grew from 8.4% to 15.2%. This stability means a very experienced labour force, as well as one that is in a position to demand some rights in terms of pay and benefits. But it also has consequences for the health of this labour force, especially under current reform conditions as the section on health makes clear. And it has consequences for the future heath human resource planning, as large numbers look forward to retirement. Moreover, it should be noted that just as the work is becoming more intense with health care reforms focused on doing more with less, those who are providing care are much older than in the past.
Table 4: Age Group Concentrations by Occupations in Health Care and Social Assistance, SLID 1993 & 2009
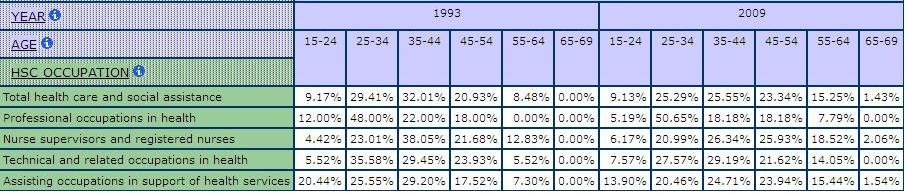
Chart 3: Visualization of Age Group Shares among Nurses, SLID 1993 & 2009
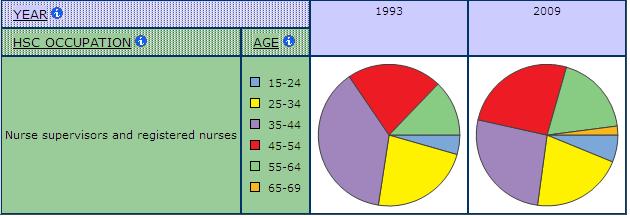
Chart 4: Visualization of Age Group Share among Nurses with Data Labels, SLID 2009
DEMONSTRATION 2
Public and private care
Canada has a complex health care system and it is necessary to understand this complexity in order to understand health care work.
Under the 1984 Canada Health Act (CHA), health care is primarily a provincial/territorial responsibility. The federal government still screens immigrants, provides care to First Nations and Inuit peoples and the armed forces and the RCMP, and regulates for drug and food safety, but most of the rest is left to the provinces and territories. Nevertheless, the federal government has used its ability to raise money through taxes as a way to influence public health care in Canada. This influence is most obviously evident in the Canada Health Act and related financial arrangements.
According to the CHA, all medically necessary services provided in hospitals and by doctors or nurses paid under the provincial/territorial plans must be universal, accessible, comprehensive and portable. Some aspects of extended care services are also covered. In addition, the government insurance plans must be administered by a non-profit, public agency. These principles are not defined in much detail. However, it is made clear that services must be provided under uniform terms and conditions and that a wide range of services are covered under the definition of hospitals, including all drugs and tests as well as all cleaning, food and laundry provided in them. The federal government, then, pays a portion of the costs of services provided under provincial jurisdiction but does not deliver them. The provinces in turn pay for services delivered primarily by agencies that are not directly government-owned. Thus, even at the height of the welfare state, Canadian health care remained mainly private in terms of delivery but public in terms of payment.
This approach to public care has a number of consequences. First, and most obviously, public health care services expanded enormously as they became more accessible to those who previously could not afford them. This expansion meant jobs in health care grew as well, especially for women. Second, services became more equally distributed not only among individuals but also across jurisdictions. Greater equity was, and is, particularly important to women and minority groups who need the system more but have fewer resources to use for payment. Third, although there was a more uniform approach, provinces and territories continued to have a great deal of leeway in determining what services are provided and how they are provided. As a result, there are considerable variations among jurisdictions in terms of such things as length of stay in hospital and number of doctors per capita. Fourth, doctors’ power grew along with the health care system in large measure because they determined what doctor or hospital care was medically necessary and thus covered by the public system. Fifth, the emphasis was on doctor and hospital care because these were the services most clearly funded by the federal plan. Other services, such as homecare and drugs provided outside hospitals, remained largely private financial responsibilities and ones that were often privately delivered, even though the Canada Health Act does mention extended health care services. Sixth, most facilities remained as non-profit, non-government institutions, albeit ones considered as part of the public sector and heavily regulated as well as funded by the various governments.
Over the years since the federal government introduced what we call medicare, it has reduced the amount of money available to provinces and territories at the same time as it has made the federal contribution significantly more difficult to calculate. The lack of clarity about how much the federal government contributed to health care combined with reductions made it more difficult for the federal government to use its financial clout to enforce the five principles of the Canada Health Act. Provinces and territories increasingly challenged the federal government’s right to a say in public care. Facing rising costs and falling federal contributions at the same time as they began embracing neo-liberal strategies, most provincial and territorial governments turned to privatization as a means of reforming public care.
In recent years, the federal government has started to make up for some of the money lost to health care under the CHST, partly at least in response to public pressure. But it has not used this increase to enforce the principles of the Canada Health Act and most provinces and territories continue to resist any such move. The federal government has now moved to a Canada Health Transfer that identifies money going to health and has increased the funding, but there is still no evidence of enforcement. The Conservative Government has announced future cuts to the Canada Health Transfer, an end to equalization payments and plans to tie the funding to economic growth, a strategy that will significantly reduce money going to the provinces. Meanwhile, the move towards privatization continues, especially in terms of for-profit delivery and methods of work organization (Armstrong and Armstrong 2003; Browne, Crossman and Fudge).
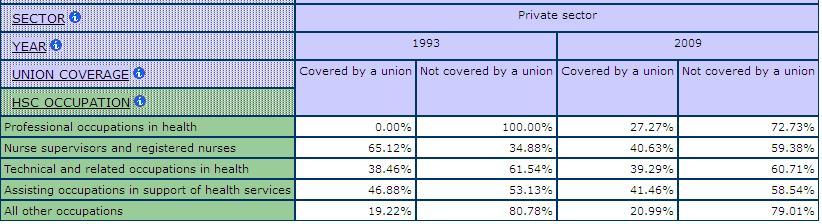
Privatization in health care takes a variety of forms (Armstrong, Armstrong and Connelly 1997; Armstrong et al. 2002). One form is the shifting of costs to insurance companies, families and individuals. Fewer services are covered under the public system and more of the public ones involve charges. Another is the adoption of for-profit managerial strategies within the public system. Such strategies include total quality management and other methods designed to reorganize work as a means of reducing the mainly female workforce. They also include approaches intended to shorten the length of stay in public care and limit the kinds of care provided under the public system. A third form of privatization, linked to the other two, is the shift of both responsibility and work to the community and the private household. This primarily means a shift to unpaid care done mainly by women. And finally, there is the move to have more of the public services delivered by for-profit agencies. Each form of privatization has consequences for the labour force in general and for the female-dominated health care work force in particular. For example, the shift to private responsibility can mean workers are reluctant to leave jobs which provide them with insurance coverage that will make up for the deficits in public care. Drugs covered by an employer’s plan could be too expensive to handle without insurance. At the same time, more women feel pressured to leave their paid work in order to provide care for their disabled children, sick partners or frail parents. Those with paid work in care face the risk of job or benefit loss and work intensification. Also impacted are the levels of union coverage and the pressures on the collective bargaining of health-related benefits (See Table 6 below on changes to union coverage by public/private and occupational classifications).
So why is this history relevant for studying health care work? Perhaps most obviously, context matters and health care is the context of the work considered here. This complex system of what Canadians think of as public care makes categorization difficult and analysis confusing. Governments pay for most of hospital and doctor care, as well as for a variety of other services depending on the province. So payment is public. This public payment makes care more accessible than it is in the United States and more efficient because it significantly reduces administrative costs. However, most delivery is private in the sense that government does not own all the hospitals or doctors’ offices, although there is some government ownership. Yet these organizations are delivering government services and are highly regulated by the state. Indeed, using a definition of public sector based on funding rather than ownership, Statistics Canada counts hospitals as part of the public sector. Some provinces own some of their long-term care facilities or their clinics or their homecare services, while others contract out these services to for-profit or not-for-profit organizations or fail to provide many of these services through the state. Not only is the system complex to start with but massive reforms are changing the location and structure of care services. This too has profound consequences for work and employment relations.
Less obviously, whether facilities are public, private not-for profit and private for-profit makes a difference in terms of how the work is structured and organized. Ownership is integrally related to decision-making and accountability. Public facilities are responsible to governments and ultimately to citizens, creating at least the possibility for transparency and democratic control. Private organizations are responsible mainly to their members or their shareholders, making it possible to claim that much of the decision-making should be kept confidential and exclusive to those members of shareholders. When organizations need to make a profit over and above what they receive in funding, there is greater pressure to reduce costs. Given that by far the greatest expenditures in health care are labour costs, the pressure to reduce both the number of workers and their wages and benefits is greater.
Finally, reforms in health care reflect the growing move towards neo-liberal practices. Shifting responsibility to the private sector and individuals, partnering with the private, for-profit sector are all patterns linked to this approach. And all these practices have profound consequences for work in care.
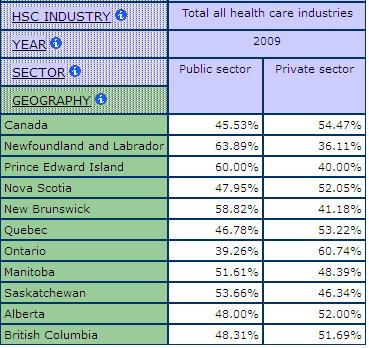
The only measure we have in the GWD to look at privatization is one that divides the labour force into public and private. Lacking are data on the for-profit and not-for-profit sectors, a limitation of labour force data available at Statistics Canada. Table 5 shows how concentrations of workers in the public and private sectors vary by provincial jurisdiction in Canada. For example, in 2009, out of all workers in health care and social assistance in Canada, 45.5% worked in the public sector compared to 54.4% in the private sector. Public sector concentrations are highest in Newfoundland and Labrador. Private sector concentrations are highest in Ontario, at 60.7% in 2009.
Table 5: Shares of Workers in the Public and Private Sector, Health Care and Social Assistance, SLID 2009
Looking at sub-industry in health care and social assistance allows us to examine some aspects of privatization. Chart 5 shows the growth of the labour force in the public and private sectors in Canada between 1993 and 2009. Chart 6 shows the growth within the sub-industry of ambulatory care. Chart 6 clearly demonstrates a much more significant growth in the size of the private sector labour force in this sub-industry where medical home care is classified.
Chart 5: Numbers of Workers in Public and Private Sector, Health Care and Social Assistance, SLID 1993-2009
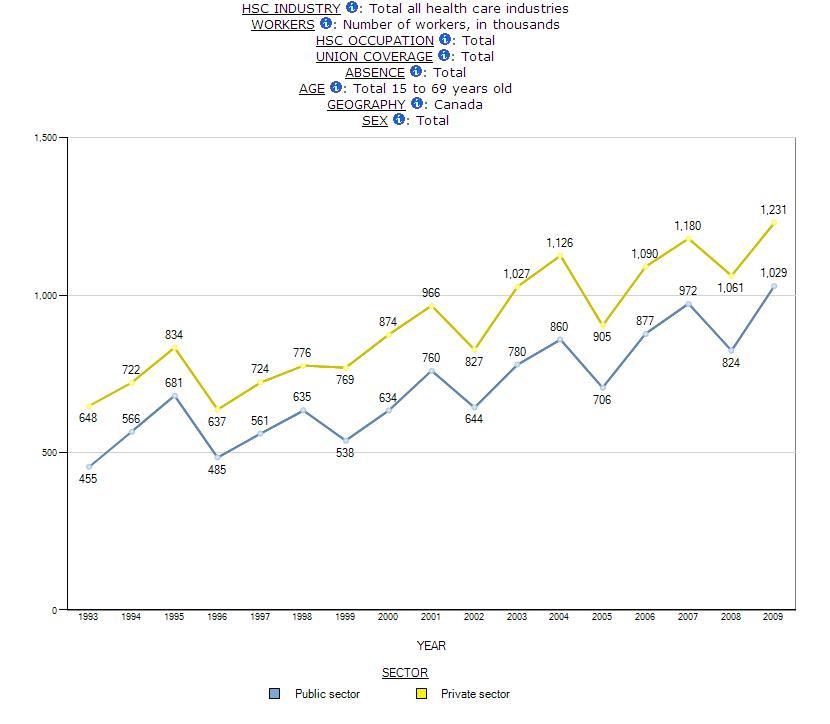
Chart 6: Numbers of Workers in Public and Private Sector, Ambulatory Care, SLID 1993-2009
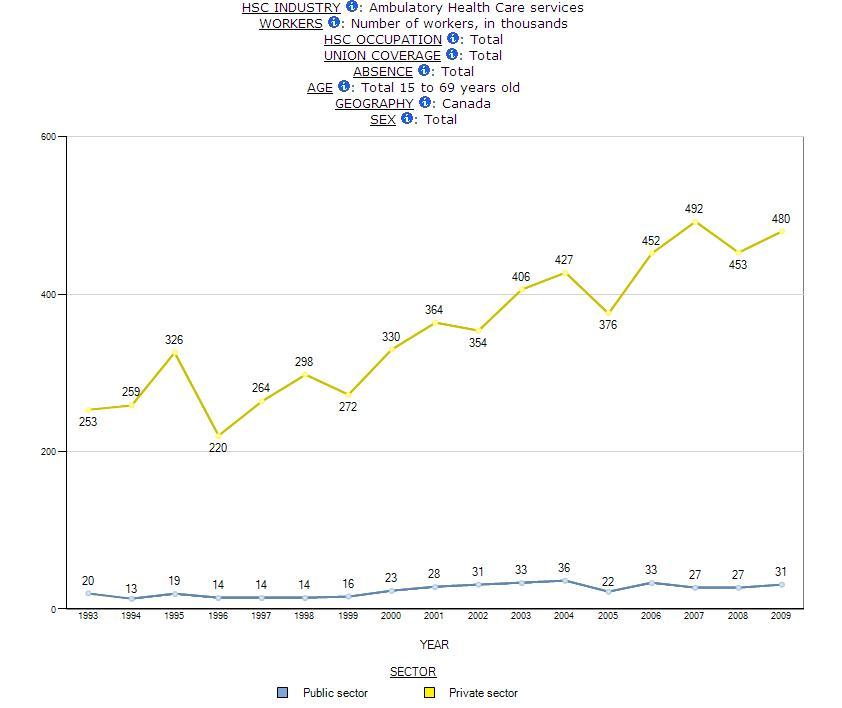
Table 6: Union Coverage, Public and Private Sector by Occupations, SLID 1993 & 2009
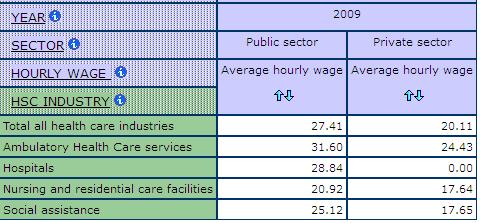
Wages are lower for workers in the private sector and many see a decline in their wages when their work is privatized. Table 7 shows the average hourly wages for workers in the public and private sector sub-industries in health care and social assistance. In 2009, workers in all sub-industries reported higher hourly wages in the public sector than in the private sector. For example, in public ambulatory, workers earned an average hourly wage of $31.60 but only $24.43 in the private sector. Workers in social assistance earned an average hourly wage of $25.15 in the public sector but only $17.65 in the private sector.
Table 7: Average Hourly Wages, Public and Private Sector, Sub-Industries in Care, SLID 2009
Statistics Canada does divide the workforce into public and private sectors, although the “funding” definition which classifies workplaces as public if publically funded does not always coincide with popular notions of public and private. Table 8 and Table 9 show the relative size of the labour force in the public and private sectors in different sub-industries and occupations in health care and social assistance. Hospitals are basically all public. Ambulatory is mostly private. Most professionals and physicians are classified as private and while most nurse supervisors and registered nurses are classified as public. These concentrations reflect where providers are working: most doctors are in private practice while most nurses are in hospitals but both are paid from the public purse and do not charge individuals for most services. Overall, however, these concentrations demonstrate the limitations of the measure for sector in Statistics Canada labour force surveys.
Table 8: Relative Size of the Public and Private Sector by Sub-Industry in Care, SLID 1993, 2000 & 2009
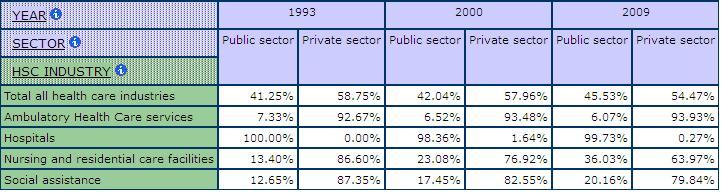
Table 9: Relative Size of the Public and Private Sector by Occupation in Care, SLID 1993 & 2009
The structure of workplaces
Workplaces in the health sector, then, are not only complex and varied. They are also undergoing significant changes. They range from single person offices to giant organizations with multiple campuses. Some are for-profit, such as many of the nursing homes; others are non-profit, such as hospitals and the Victorian Order of Nurses. The non-profit sector is itself divided into two kinds of organizations. One encompasses quasi-autonomous, non-governmental organizations or quangos. Hospitals fall into this category because, like schools and universities, they are so highly regulated and funded by governments that they can be considered almost part of government. The other kind of non-profit organization is often called the voluntary or the third sector or simply the non-profit one, distinguishing them from the quangos. Family services, residential care facilities and day care all fall into this latter category when they are non-profit. As with other classificatory distinctions, however, this one needs to be used cautiously. Non-profit organizations receiving any public funds are increasingly subject to uncertain, project-based funding while constrained by narrow, quantified outcome requirements and restrictions on their advocacy activities (see, for example, Woolford and Curan 2011)
In 1999, Statistics Canada conducted the Workplace and Employment Survey (WES) which provided a picture of quango and non-profit workplaces compared to for-profit ones. As McMullen and Brisbois (2003: vi) point out in their analysis of the data in WES, the survey was limited by the business perspective based on a for-profit model and by the failure to count either workplaces run entirely by volunteers or those volunteers who work beside paid workers. Nevertheless, McMullen and Brisbois used the WES to develop a picture of the workplaces and employees in ways that allow comparisons among the three groups. The neo-liberal ideas reflected in the new public management strategies have helped make quangos and non-profits look more like the for-profit sector. Indeed, that is their purpose. Increasingly, governments in Canada seek to make all organizations operate as they think business operates. At the same time, the neo-liberal philosophy and practice seek to reduce government involvement in service delivery, shifting more of the work to the non-profit sector and volunteers. Although these strategies have had a profound impact throughout the sector and forced some harmonizing in approaches, significant differences remain among the for-profit, quango and non-profit organizations. According to the WES, large workplaces are most common in the quango sector, with two-fifths of the establishments employing 50 or more workers and 97% of employees working in such places. Small workplaces are much more common in both the non-profit and for-profit sectors, with only about 15% employing 20 or more workers. However, workers were more concentrated in large establishments.
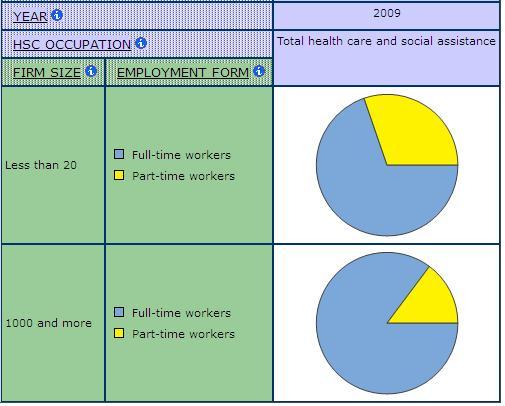
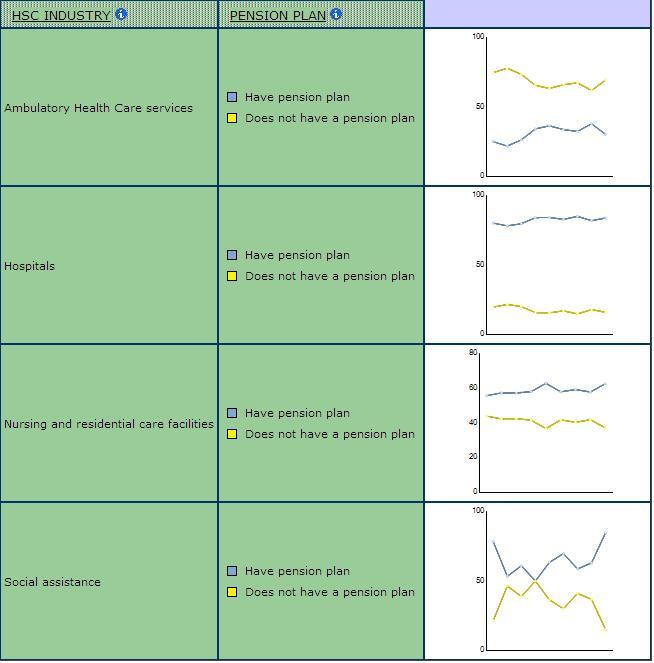
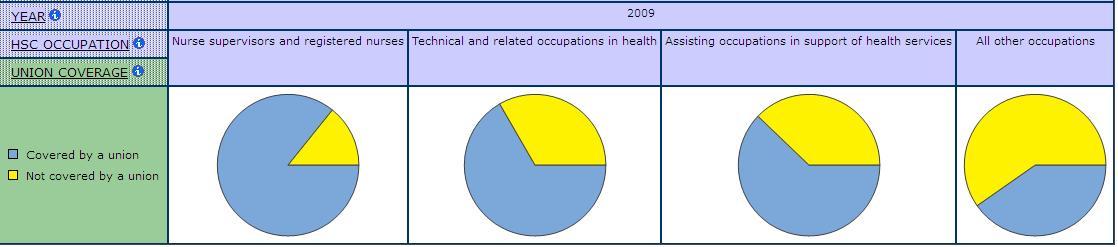
Size can influence the extent to which people have control over their work as some labour regulations apply only to large workplaces. Unions are also more likely in larger establishments, and unions help protect workers from infringements of their rights (Chart 7). Moreover, for-profit organizations “tend to be governed by a strongly hierarchical, top-down management model” (McMullen and Brisbois 2003: vii) while non-profits are more likely to allow employees greater involvement in decision-making. However, non-profits are more likely to have their decisions restricted by forces outside their organization, such as the funding rules of governments. As Chart 8 shows, hourly wages are lower in smaller establishments than in larger ones in health care and social assistance. There is also a larger share of part-time employment in smaller firms in care (Chart 9).
Chart 7: Union Coverage by Firm Size, Health Care and Social Assistance, SLID 2009
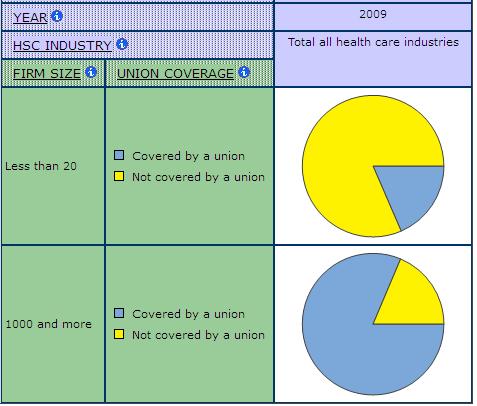
Chart 8: Hourly Wage by Establishment Size, Health Care and Social Assistance, SLID 2009
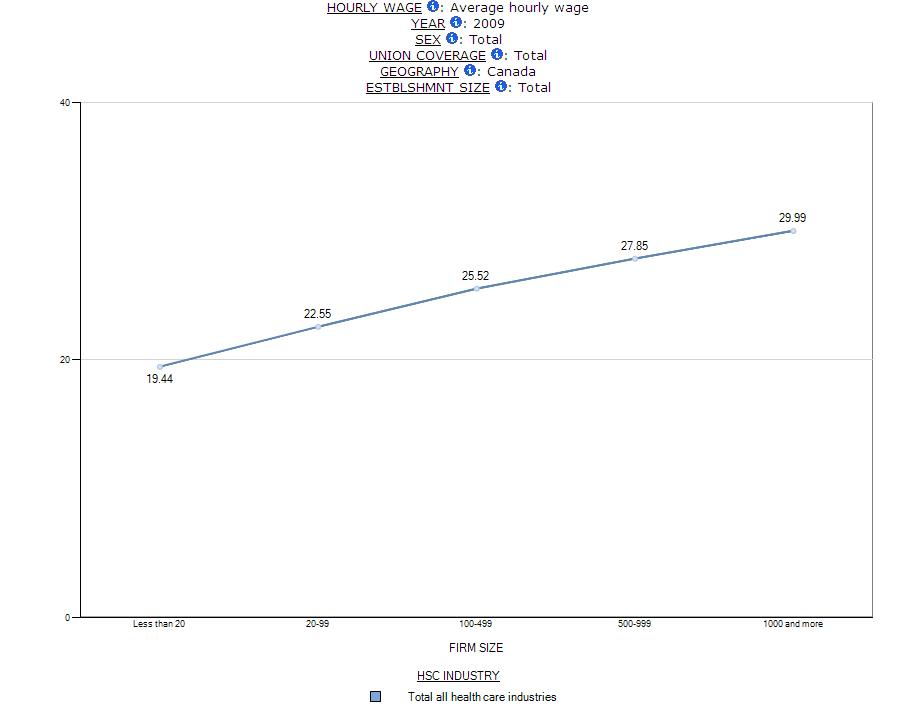
Chart 9: Full-time and Part-time Employment by Firm Size, Health Care and Social Assistance, SLID 2009
Given the link to unionization, it is not surprising that large organizations are also more likely to provide better benefits. For example, pension coverage is much higher in hospitals than in ambulatory care where smaller workplace dominate (Chart 10)
Chart 10: Pension Coverage by Sub-Industry in Health Care and Social Assistance, SLID 2009
Health care workplaces, then, are enormously varied. Most people work in large establishments, especially if they are employed in the quango sector. These large workplaces are the ones most likely to be unionized and to be subject to health and labour standards. At the same time, a significant number of workers are employed in the private sector where union coverage and other protections are less likely. This is particularly the case for ancillary workers.
DEMONSTRATION 3
Professions and unions in care
Workers have been organizing to defend and protect themselves for well over a century in Canada. Agriculture and other forms of independent commodity production dominated the nineteenth century Canadian economy. Such forms are not very fertile grounds for collective organizing, although certainly farmers formed cooperatives and fishers joined unions in the twentieth century. However, the nineteenth century did see unions organized in the developing goods production sector and in primary extraction industries. Men formed the large majority of the labour force in these sectors. Women nevertheless joined unions in the garment industry and in other production sectors where they found work, in spite of the barriers they faced from the law and from men.
The men who worked as doctors also have a long history of organizing to ensure and protect their work. Most of them were self-employed, and they used their organizations to establish shared practices and fees, to determine who could become a member and what they needed to know, to negotiate with those who paid or attempted to regulate them, and to develop collective benefits and services. They organized on the basis of what they defined as professions, distinguishing themselves from unions. Like craft unions, they are united on the basis of their skills rather than their workplaces, as is the case with industrial unions. Unlike craft unions, however, professions see themselves as united by particular intellectual disciplines that are taught in universities, based on theory and motivated by altruism. There is a great deal of debate both about what particular traits characterize a profession and about whether such characteristics are primarily the reason for their power or a justification for their power (Freidson 1970; Johnson 1972). And there are issues to be raised about the gendered nature of both professions and the analysis of professions (Armstrong 1993; Armstrong and Armstrong 1992; Witz 1992). What is clear is that their success in requiring a university education and in controlling entry meant the professions were long dominated by white men with access to economic resources.
Women who worked for pay in health care took longer to organize, in part because they were women. Almost all of them were called nurses and they were outnumbered by doctors a century ago, although these official counts probably left out the many women who worked as lay nurses (Coburn 1987). Most of these nurses worked in private homes, unless they were members of the religious orders that provided most of the institutional care. The combination of scattered workplaces, religious commitments and ideas about women’s place made it difficult to organize. So did employer practices that required women to leave paid work once they married. The Nightingale tradition also played a role. Nightingale schools were established in the late nineteenth century Canada and followed notions of female obedience and military order. As Judi Coburn has made clear, the nursing schools sought “the instilment of strict authoritarian values,” a stance evident in the motto “chosen for the first school of nursing: ‘I see and am silent'” (Coburn 1987:447-448).
Nevertheless, nurses did start to organize. When they did start, it is not surprising that nurses sought to follow the male lead and look for recognition as a profession. Not only were doctors the model in health care but doctors also had considerable power, authority and income, all of which was attributed to their professional status. Following the doctors’ lead, the nursing graduates formed the Canadian National Association of Trained Nurses in 1908. This professional organization sought to encourage “mutual understanding and unity among nurses in Canada” (Mussallem 1988:401), elevate “the standards of education and promotion of a high standard of professional honor and establish a code of ethics” (Jansen 1988:460). Like doctors, they struggled to ensure the legislative regulation of their profession. However, the first mandatory regulation was not introduced until 1953. And like the doctors, they worked to make a university education a requirement for recognition as a registered nurse. This too has taken much longer than it did for doctors and only recently have most provinces adopted policies that move in this direction. Not all nurses are happy with this development, in part because it follows the doctors’ pattern rather than stressing the unique approach of nursing work and in part because it requires more economic resources, limiting entry by marginalized groups (Armstrong and Silas 2014).
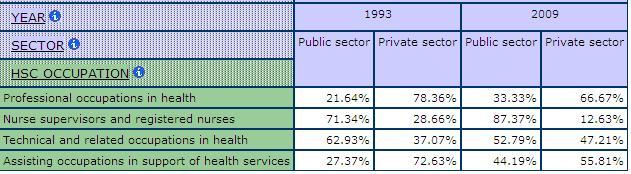
By the 1940s, the RNs were represented at the national level by the Canadian Nurses Association (CNA). Although the CNA supported collective bargaining for nurses, it insisted that it remain a professional organization and that there be no strikes. But a 1970 ruling in Saskatchewan argued that the provincial organization could not act as a union because it included nurse-managers on its board. From this point on, nurses’ unions began to emerge and to act much more like other unions. Today, over 80% of employed nurses belong to unions (Chart 11).
Chart 11: Union Coverage by Occupation in Health Care and Social Assistance, SLID 2009
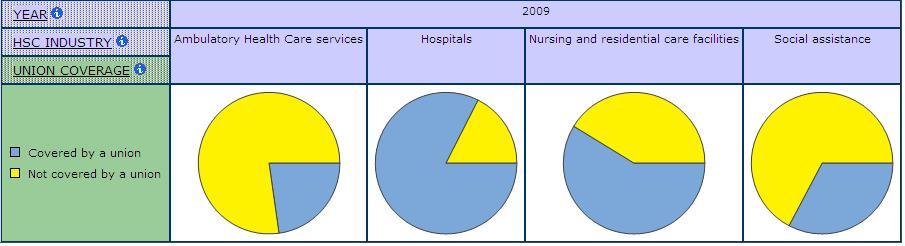
Union organizing was facilitated by the federal funding of first hospital construction and then hospital care. Nurses were brought together in large workplaces where their shared time and experiences made organizing easier. Chart 12 shows the very high level of union coverage in the hospital industry relative to the other sub-industries in health care and social assistance, reflecting some of the advantage unions have had in organizing larger workplaces in health. The movement of nursing education out of hospitals also helped, because nurses were less subject to the daily discipline and cultural traditions of nursing at the same time as they were more exposed to the challenging critiques developing in post-secondary institutions. The women’s movement also helped, especially in terms of its successful demands to allow women to stay in their paid jobs after marriage and childbirth.
Chart 12: Union Coverage by Sub-Industry in Health Care and Social Assistance, SLID 2009
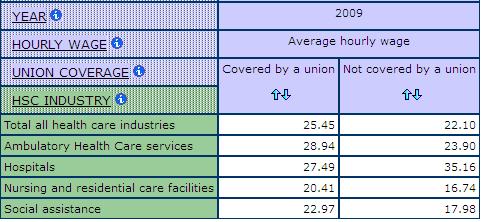
The combination of the growth in hospital size and the nurse unions’ successes in demanding better pay and conditions contributed to the increasing fragmentation of nursing work. So did the development of technology and science, not only in medicine but also in management. More of the work previously done by nurses is now done by others. Some, like the therapists and technicians, defined themselves as professionals and organized on that basis. But most, like nursing assistants, personal care providers, cleaners, dietary aides and launderers defined themselves as workers and started to organize their own unions. By the 1980s, the majority of these workers too belonged to unions. As a result, wages improved significantly, indeed Table 10 shows higher average hourly wages in unionized jobs than non-unionized in all sub-industries in health care and social assistance except hospitals. Benefits such as vacations, pensions and extended health insurance were introduced and expanded. Jobs became more secure, as did hours of employment. The success of these unions and professional organizations has contributed to the rising costs of health care, especially given that health care is highly labour intensive and that much of the care work in the past was done by low paid or unpaid nurses.
Table 10: Average Hourly Wages by Union Coverage and Sub-Industry, SLID 2009
Strategies designed to address rising costs have varied somewhat from jurisdiction to jurisdiction. However, they have primarily focused on the labour costs of the largely female workforce. Some governments began by seeking wage controls. More commonly, new managerial approaches taken from the for-profit sector were introduced to reduce both patient stays and the amount of care each patient received. Regulations were changed or removed. For example, the Ontario government eliminated the requirement that each patient in long-term care receive a minimum of 2.5 hours of nursing care each day. Hospitals were amalgamated to reduce staff numbers. Some were even closed. More people were hired on part-time and short-term contracts or from agencies as a way of increasing staffing level flexibility and avoiding expenses such as benefits. More care has been shifted to long-term facilities and to households.
And some work has been privatized. This is especially the case with the so-called ancillary workers. When the work is contracted out, former employees may lose their jobs and/ or their unions. They may also lose their rights to protection from aspects of the labour law. Similarly labeled jobs in the for-profit sector are less likely to be unionized and, partly as a result, less likely to have decent wages and working conditions. Table 11 shows some decline in union coverage for nurse supervisors and registered nurses between 1993 and 2009.
Table 11: Union Coverage by Occupation in Health Care and Social Assistance, SLID 1993 & 2009
Even those workers who have remained employed in the public sector and have remained union members have experienced a deterioration in their employment relations and conditions of work. The number of full-time, full-year nursing jobs has plummeted. Wages and benefits have failed to keep up. Unions representing registered nurses have enjoyed some success in demanding better wages and conditions as well as a strategy to address future demands. But other workers in health care have been less successful. This is especially the case in the areas where it is assumed any woman knows how to do the work and where visible minority and immigrant women are found in significant numbers.
While the majority of those defined as working in the health care sector are still covered by collective agreements, there is no guarantee that this will continue to be the case. Indeed, reforms seem to be designed to ensure this is not the case. Hospitals are most likely to be unionized and within them, the direct care providers are also the most likely to be unionized. The farther care moves away from hospitals and direct providers, the less likely union coverage.
DEMONSTRATION 4
Social reproduction
Health care is not only provided in formal institutions. It is also provided in households and communities. How much care is provided by whom and what kind of care they provide is difficult to determine, in large measure because so much of it is unpaid and performed by women.
Statistics Canada has attempted to count this unpaid labour, although there remains no internationally recognized definition of unpaid work (Macredie and Sewell, 1999). Several surveys collect relevant data but the most detailed are those produced by the time-use diaries that are the basis for the General Social Survey (GSS). Participants in the GSS recorded the start and end time for each of their daily activities, with interviews also conducted over a twelve month period. However, significant problems remain with the data that result. Statistics Canada did collect data on unpaid work in the Census, but this was discontinued in the 2011 Census.
One of the problems is the invisibility of work in households and the traditional division of labour there. The invisibility is linked both to the privacy of homes and to the unpaid nature of domestic work, as well as to the association with women. Women have long taken the major responsibility for cooking, cleaning, laundry, shopping and caring. When people become ill, disabled or frail, the workload in the household increases but the ongoing labour, along with the additional work, frequently seem to be just part of what women do. As a result, when women are asked to calculate the time spent on care, much of it may be invisible to them and thus unrecorded in surveys. In contrast, men are more likely to record their care workloads precisely because it is non-traditional work for them. Moreover, care time is very difficult to calculate because it has both multiple dimensions and overlaps with so much of women’s other work in the home. Indeed, women often do many tasks simultaneously. Counting all their tasks makes their time calculations total more than 24 hours in a day. The alternative of counting only the primary task understates the range of work they do each day.
Although the data are far from precise, they do reveal some obvious patterns. As daughters, mothers, partners, friends, or as volunteers, women are the overwhelming majority of unpaid primary caregivers and spend more time than men in providing care. Women are also the overwhelming majority of the volunteers who provide unpaid personal care to non-family members.
Women not only put in more hours than men. Women are also much more likely than men to do personal care and offer emotional support. According to the data from the General Social Survey, 21 per cent of women compared to 11 per cent of men are involved in the physical care of children. Women also provide 120 of the 190 million hours per year devoted to personal and other care for adults. And women provide twice as much care for the ill or disabled and more than three times as much unpaid babysitting (Zukewich 2003: 17). Men’s contributions are more likely to be concentrated in care management or household maintenance, shopping or transportation (Campbell and Martin-Mathews, 2000; Rosenthal and Martin-Mathews 1999). In other words, women are more likely to provide the care that is daily and inflexible while men provide care that can be more easily planned and organized around paid work (Gignac, Kelloway and Gottlieb 1996). And men are more likely than women to get formal help when they do provide care, on the assumptions that they must have paid jobs and that they lack the skills necessary to provide care (Aronson and Neysmith 1997; Morris et al. 1999; Keefe and Fancey 1997). Yet women provide personal care even when they have paid jobs, although higher income women may be better positioned to become care managers, rather than care providers (Rosenthal and Martin-Matthews 1999). In spite of this evidence documenting a significant division of labour between women and men, the most recent “Portrait of Caregivers” from Statistics Canada simply compares the overall numbers of women and men reporting they are involved in any of maintenance, transportation, domestic support and personal care (Sinha 2012). Similarly, another Statistics Canada publication (Turcotte 2013) on the consequences of caregiving fails to analyze the data by gender even though other evidence (Duxbury and Higgins 2012) suggests women face more negative consequences in part because of the nature of the care they provide.
Some men have to, and continue to, provide care in a variety of forms. Like women, they care for their spouses. However, fewer men are called on for such care because their wives usually outlive them, given women’s greater longevity and the pattern of men marrying women younger than themselves. Men care for their parents too, providing up to a quarter of this care (Campbell and Martin-Matthews, 2000). Men also care for their same sex partners, and serve as volunteers who manage care, provide transport and support, deliver meals and do household chores. And like women, men may provide care to siblings, in-laws or other relatives (Buchignani and Armstrong-Esther 1999). Data in the GWD from the 2006 Census show the average hours per day spent on various unpaid activities for men and women (Table 12). Women’s total unpaid average hours per day are 4.19 compared to 2.78 for men. Women do more domestic work than men, they also do more care giving both to people in their own household and to people outside their household. Women are also more likely than men to report being absent from work in order to care for others (Table 13).
Table 12: Average Hours per Day on Unpaid Activities, Men and Women, Census 2006
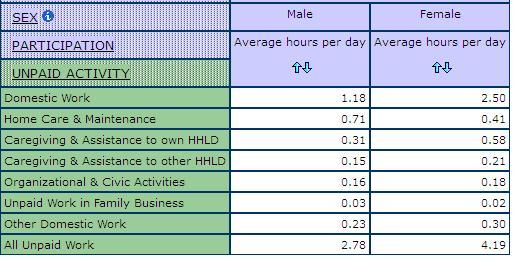
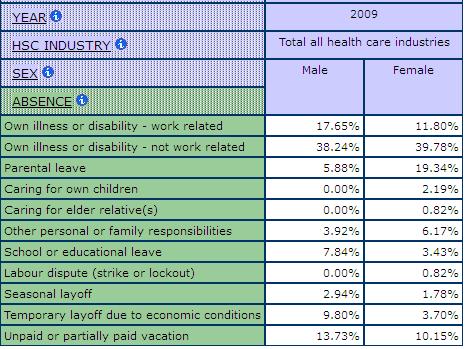
Table 13: Reasons for Absence from Work, Men and Women in Health Care and Social Assistance, SLID 2009
Friends also provide considerable care, although we know less about them than we do about the spouses, mothers and children who are caregivers. A Statistics Canada study found that nearly one in five of those who had moved in order to provide care were friends, rather than relatives, suggesting that friends do much more than offer the occasional visit (Cranswick 1999: 12).
In addition to family and friends who provide care, there are also volunteers who offer various kinds of support. Statistics Canada does record volunteering, distinguishing formal volunteers who work through organizations from those informal volunteers who simply offer their time or money on their own. As is the case with unpaid caregiving, it is important to assess what kind of volunteering is being recorded and what kinds of hours are spent volunteering. Statistics Canada counts a very wide range of activities as volunteering, many of which are quite remote from care work broadly defined.
Volunteers are most commonly found in the arts, culture and recreation industry. “In 2010, 12% of people aged 15 and over did volunteer work for sports and recreation organizations and 12% for non-profit organizations providing social services; 10% devoted their time and energy to associations engaged in education and research, another 9% to religious organizations, and 6% to those supporting health issues” (Vezina and Crompton 2012: 39). However, twice as many people provide informal direct care, compared to those who volunteer in formal organizations, with 53% of them providing health related personal care (Vezina and Crompton 2012: 51). In other words, volunteering is not primarily about providing care but a significant number of people do volunteer as caregivers. Past research indicates that women are more concentrated than men in the volunteering work that takes long hours and in volunteer work that involves direct care. Although Statistics Canada’s (Vezina and Crompton 2012) latest report on volunteering provides analysis of data by age, education, parental status, employment, it does not tell us what proportion of those volunteering to provide unpaid care as women.
Similarly, the report indicates that more young people are volunteering, a change that can partly be explained by school regulations in some parts of the country that now require students to do such work (Vezina and Crompton 2012: 40). However, we are not told whether young women are more likely than men to volunteer.
Some employers allow volunteering on company time (Statistics Canada 2012b). The most common types of employer support are use of facilities, timeoff and flexible hours intended to accommodate volunteering (Luffman 2003). However, here too it is important to note what is counted as volunteering. Almost two thirds of unionized workers (63%) reported use of facilities as the most common form of support while non-unionized workers mostly reported time off work (Luffman 2003: 1). Given the wide range of activities included as volunteering, it is difficult to tell how many employers allow time or support to care.
Thus, in assessing care, it is not only important to ask who provides care. It is also necessary to ask what kinds of care they provide, for whom and how often.
Equally important, we need to ask what kinds of options providers have in terms of providing this care. The research that has been done about differences among women caregivers suggests that income and education matter at least as much as culture in terms of the kinds and amounts of care provided and thus in the choices women have (Chubachi 1999; Decima Research Inc 2002; Dorazio-Migliore 1999; Guberman 1999, 2004). Women with money are more likely to have the means to purchase care and often do so, regardless of their cultural background or immigration status. And the poorer women are, regardless of their culture, the more likely they are to have little choice about providing care (Morris et al. 1999; Armstrong 2013). Women told the National Forum on Health (1997:19) that most women want to provide various kinds of informal care but few want to be “conscripted” into this relationship.
Some cultural groups are also much more likely than others to live in households that hold several generations, suggesting cross-generational caregiving. But this is not necessarily the case. While for example East Indian immigrants tend to live in multi-generational households, it is important not to assume that this, like the lower use of formal services, simply indicates cultural choices. This pattern may be as much about immigration regulations requiring support for sponsored relatives and limited economic resources as it is about preference (Dhawan1998). For example, the evidence that Chinese, Greek and Italian elderly are less likely to live alone than are other Canadians may reflect low incomes, lack of pensions and immigration rules as much as cultural values (Brotman 1998). Similarly, the fact that Aboriginal seniors are much more likely to live with relatives than are other Canadians may reflect poverty as much as choice or values (Buchignani and Armstrong-Esther 1999).
Like sponsored immigrants, spouses face rules governing support. The rules are fairly clear in terms of financial support, but less clear when it comes to providing direct care services. It is not evident that spousal support means you could take your partner to court to demand they change your diapers, insert your catheter or attach your oxygen mask. Certainly many of the policies and regulations in health care assume such support, especially from women, and enforce it through a failure to provide alternatives or through regulations. In Ontario, for example, each Community Care Access Centre determines eligibility for homecare and may use its own criteria to assess whether families can provide the support required. Who constitutes a family for the purposes of providing such care is not clear, however, and given assumptions about women’s caring family often means women.
Children also can face legal obligations for support of their parents. These filial responsibility laws require children to provide support if parents need support, have supported the children in the past and if the children can afford to provide support (Bracci 2000; Snell 1990). In BC for example, the Family Relations Act (RSBC 1996) CHAPTER 128 says that a child is liable for maintaining and supporting parents. Sons are more likely, given higher work wages, to be able to afford financial assistance. It is perhaps not surprising that these laws are seldom used, in part, because many sons do support their parents when they can, just as spouses and same-sex couples and friends do. When they cannot meet this responsibility, or when they reject it, the enforcement of these filial laws is not very common (Bracci 2000; Snell 1990).
Employees also have legal obligations; ones that may prevent rather than promote caregiving. One in four employees provides care, and a large proportion of care providers is employed (MacBride-King 1999). Not surprisingly, those with both eldercare and childcare responsibilities, most of whom are women, are the most likely to lose time at work as a result of caregiving (Cranswick 1999: 12). The most heavily involved in caregiving are likely to withdraw from the labour force as a result (Lilly, Laporte and Coyte 2007). The very limited leave allowed for such care, combined with very few protections from being fired when caregiver stress leads to missed time at their paid jobs, mean that caregivers are very vulnerable at work. Those who care for people unrelated by blood or marriage may be particularly at risk.
Lack of job security and other kinds of precariousness in the employment relationship may make it difficult for people with paid work to provide unpaid care. Irregular work hours, more common for women, makes it difficult to plan care. Nevertheless, the demand for unpaid care is increasing just as employment is becoming more precarious. The federal government has made a small move to support some unpaid care providers under Employment Insurance (EI), but this is very limited support and many women may be ineligible for the benefit, given that they may not have the hours of paid work required for EI qualification. There are also limited tax benefits available. Some unions have negotiated leave arrangements that can be used to care for ill relatives.
Finally, any discussion of unpaid care must consider skill. Very little research has been done on the skill level of such care providers and there is very little evidence that providers are tested for skills. Statistics Canada’s survey of volunteers (Vezina and Crompton 2012: 48) found that “about two-thirds (64%) said their interpersonal skills had improved…Volunteers also thought their volunteer experience had given them better skills in communications (44%), organizing (39%), fundraising (33%) and technical or office work (27%). One-third (34%) also reported that working as a volunteer had increased their knowledge of such subjects as health, women’s or political issues, criminal justice or the environment. Yet we could find no similar data on family members who provide the bulk of unpaid care. This failure to ask about these skills reflects that assumption that women in particular have the skills to care and the desire to do the work, along with the moral obligation. Some short training is sometimes provided by nurses and others. But nurses find themselves teaching women family members how to do tasks the nurses have taken entire courses to learn. The process makes the skills of all those involved less visible and, ultimately, less valued.
In short, most women take major responsibility for the care work that goes on in the home or community. Resources certainly matter, making it more possible for some women to purchase care or to get help and support with care. So do cultural practices. But gender is critical, influencing not only what care women provide at home but also the work they do for pay. However, government and employer practices are equally important because they determine to a large extent what resources or alternatives are available as well as the conditions of paid work that influence the possibilities for care (Grant et al. 2004). Measuring the extent of unpaid care work not only provides a means of making visible women’s unpaid work; it is also critical for developing an accurate account of economic production. If women did not do this work without pay, it would in many instances have to be done by someone with pay. Indeed, some at least of the current care work done in the home was previously done by paid providers.
DEMONSTRATION 5
The health of health care workers
Health care has emerged as a high-risk industry and nursing and personal care have emerged as the most dangerous occupations in health care and social assistance (Dabboussy and Uppal 2012). Part of why these occupations are so dangerous is related to the very high concentrations of women who do this work. In this demonstration we will explain why this is the case and we will showcase a couple indicators of health and well-being included within the Health Care Module.
First, because nurses and personal care providers are women, we now have a majority who are over the age of 40. This has never happened before, because they are women. Until this generation, we made women leave when they got married, and somewhat later we let them stay after marriage but made them leave when they became pregnant. As a result, nursing staff in the past were either young or single and senior, with the senior nurses much less likely to undertake regular bedside care. Nevertheless nursing work organization often still assumes young fit women are doing the bedside care. Indeed, the workload in this very physically demanding job has increased along with the age of the nurses (Armstrong and Laxer 2013).
Second, because nurses and personal care providers are women, we have not understood the work as physically demanding in the same the same way we see much of men’s labour as physically demanding. This too contributes to the failure to develop policies that adequately take these demands into account. Women have often been loath to stress the physical demands because they were trying to establish nursing as a profession and because they did not want to appear as weak females.
Third, because nurses and personal care providers are women, they feel responsible and are held responsible for care. New managerial strategies designed to shorten patient stays and provide more care on an outpatient basis have dramatically increased the pace of nursing work. The result is not only a speed-up in the work but also a severe reduction in the time available to provide the kind of care nurses have learned to provide. Nurses tell us they still scramble to make up for the care deficit and they are expected to do so. The expectations they have of themselves and that others have of them are directly linked to gendered assumptions of nursing work. Recent research has begun to recognize the health hazards created by the organization reforms but fails to link these hazards to the gendered assumptions in the work (see, for example, B.C. Nurses Union 2004; Institute of Work and Health 2011; Shamian and Villeneuve 2004: 24-25; Yassi and Hancock 2005).
Fourth, because nurse and personal care providers are women, many of the skills are assumed to come naturally. In practice, many of the skills are learned informally from other women in the process of doing the work. Such learning takes time as well as effort, but the time for continual learning interchange is disappearing as the focus on measurable tasks increases.
Finally, because they are women they are doing more than one job. When they go home at night, they take up very similar work in the household. Increasingly, they are looking after family, friends and relatives who need homecare. The pressure to provide the care that is being sent home is particularly heavy on women with direct health care experience, as we found with personal support workers in long-term residential care (Armstrong et al. 2009).
In short, older nurses and personal care providers are working much harder at a double or triple shift in ways that make them more vulnerable to illness and injury. The high rates of illness and injury are a concern not only to nurses and personal care providers but also to their patients and to the system as a whole. Injury and illness costs us all. If the absenteeism rate of RNs were reduced to that of all other workers, the equivalent of almost 5,500 more would be at work full-time each year (CIHI 2002: 87). Gender is a critical component in understanding the increases and thus in addressing these outcomes.
Similar patterns can be found throughout the female-dominated health care labour force. In the GWD we have indicators that shed some light on the health and well-being of workers in health care and social assistance. For example, we use the variable for self-reported health status from the Survey of Labour and Income Dynamics. Chart 13 shows the self-reported health status for workers in the different occupations in health care and social assistance. Among physicians and professionals, virtually no one report having fair or poor health. The distribution is much different for workers in the assisting occupations in support of health services and in all other occupations (support workers), where there are relatively high concentrations of workers reporting fair or poor health.
Chart 13: Self-reported Health Status by Occupation in Health Care and Social Assistance, SLID 2009
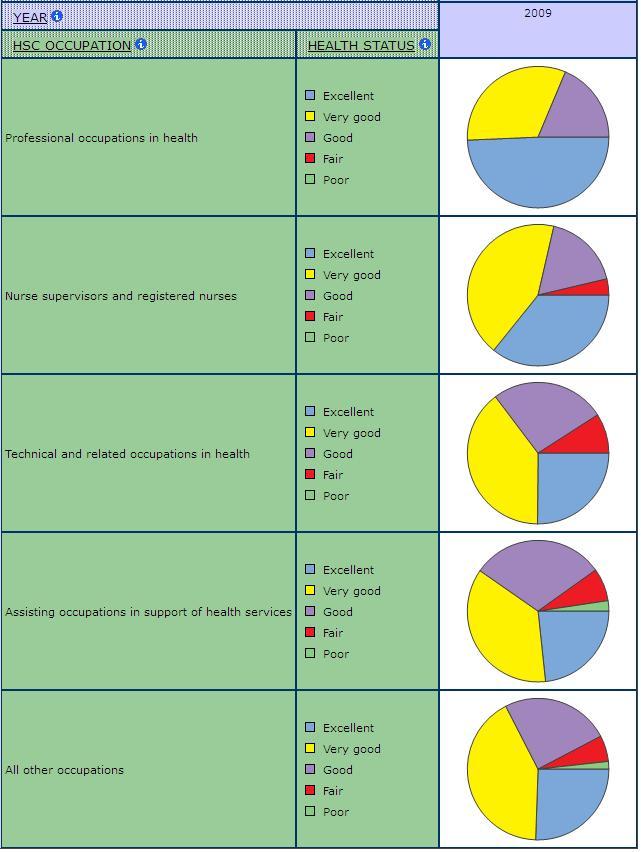
We are only beginning to produce research on the health consequences for unpaid providers. The Decima Research Survey (2002: 6) of unpaid providers found that half of them had difficulties with their emotional and physical health as a result of care work. 70% said they found that “providing this care had been stressful”. “The most significant predictor (indicator) of caregiving stress is lack of choice in taking on this responsibility”. Statistics Canada’s 2013 study of family caregivers also found significant health, financial and employment consequences for regular caregivers, as did Duxbury and Higgins (2012). Given that fewer and fewer women have a choice about providing unpaid care, we can expect stress levels and accompanying health problems to rise.
Work reorganization, health care reforms and assumptions about gender all contribute to the declining health of care providers. Also contributing is a push towards atypical shifts in care such as on-call and split shifts which help managers coordinate care according to their demands but which undermine workers’ control in planning their daily lives. There has been a growth of this sort of scheduling and some workers such as women in nursing and residential care (Laxer 2013) are more likely to work in these atypical schedules. Recent research has begun to uncover the risks of working night and rotating shifts in terms of illnesses such as cancer (see health and social care module of the comparative perspectives on precarious employment database).
Chart 14: Work Schedule in Health Care and Social Assistance, SLID 2009
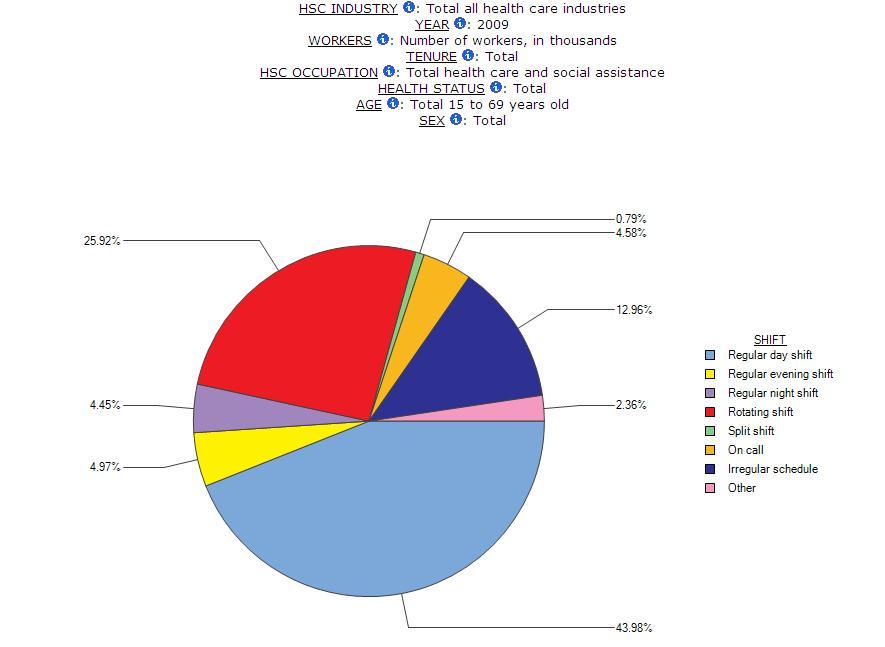
Conclusions
Women have struggled hard to make visible and valued the work and skills involved in care. And they have enjoyed some success. The establishment of a public payment system, combined with the development of large facilities, created conditions that made unions easier to organize. The women’s movement also played a critical role in terms of state policies and programs related to both paid and unpaid care.
The women who made the most significant gains were those who followed the male pattern of creating regulated professions based on formal education programs. These are the women recognized as being employed in health care occupations, as direct providers. Their success contributed to the growth of other jobs in care as more of nurses’ job went to other workers. Women in ancillary occupations also improved their conditions of work and of employment in care, although perhaps not to the same extent. At the same time, their numbers grew significantly and so did the proportions from racialized and/or immigrant groups, especially in large urban areas. Those not directly providing care, employed in support provider roles, account for the majority of the health care labour force.
Health care reforms have been fundamentally changing both the conditions and location of work. All workers, paid and unpaid, have felt the impact. For-profit managerial practices in health care services have made work more intensive and more precarious. They have also emphasized the distinction between direct and ancillary care work. This distinction has been used to define ancillary workers out of care, creating the conditions for contracting out the work and for undermining women’s gains. At the same time, more of the work has been shifted out of large hospitals into smaller, and increasingly, for-profit residential facilities where unions are harder to organize and where workers often have less power. When the work does not go to these facilities, it most frequently goes home where it is done primarily by women without pay, formal training or much choice. The result is often not only deteriorating working conditions but also deteriorating health for patients as more of those with acute care needs are put in settings not equipped or staffed for appropriate care. Statistics Canada provides the data to support many of these claims and to provide the kind of occupational, as well as historical, data that help us monitor the impact of changes. Although Statistics Canada has made efforts to track unpaid care, this has been compromised by the recent removal of questions related to unpaid work in the Canadian Census.
WORKS CITED
Armstrong, P. (1993). “Profession, Unions or What?: Learning From Nurses.” In Linda Briskin and Pat McDermott (Eds.), Women Challenging Unions. Toronto: University of Toronto Press.
Armstrong, P. (1996). “The Feminization of the Labour Force: Harmonizing Down in a Global Economy.” In Isabella Bakker (Ed.), Rethinking Restructuring: Gender and Change in Canada. Toronto: University of Toronto Press.
Armstrong, P. (2013a). Unpaid Healthcare Work: An Indicator of Equity. Pan American Health Organization.
Armstrong, P. (2013b). “Puzzling Skills.” Canadian Review of Sociology, Special Issue 50th Anniversary of the Canadian Review of Sociology, 53(3), 256-283.
Armstrong, P. (2013c). “Skills for Care.” In Pat Armstrong and Susan Braedley (Eds.), Troubling Care: Critical Perspective on Research and Practices. (pp. 101-112). Toronto: Canadian Scholars Press.
Armstrong, P. and Armstrong, H. (1992). “Sex and the Professions in Canada.” Journal of Canadian Studies, 27(1), 118-135.
Armstrong, P. and Armstrong, H. (2002). “Women, Privatization, and Health Care Reform: The Ontario Case.” In Pat Armstrong et al. (Eds.), Exposing Privatization: Women and Health Care Reform in Canada. Aurora: Garamond Press.
Armstrong, P. and Armstrong, H. (2003). Wasting Away: The Undermining of Canadian Health Care, Second Edition. Toronto: Oxford University Press.
Armstrong, P. and Armstrong, H. (2009). “Contradictions at Work: Struggles for Control in Canadian Health Care.” In Leo Panitch and Colin Leys (Eds.), Morbid Symptoms: Health Under Capitalism. (pp. 145-167). Ponty Wales: Merlin Press.
Armstrong, P. and Armstrong, H. (2010). Wasting Away: The Undermining of Canadian Health Services. Toronto: University of Toronto Press.
Armstrong, P., Armstrong, H. and Connelly, M. P. (1997). “The Many Forms of Privatization.” Studies in Political Economy, 53 (Summer), 3-9.
Armstrong, P., Armstrong, H. and Scott-Dixon, K. (2008). “Critical to Care: The Invisible Women in Health Services.” Toronto: University of Toronto Press.
Armstrong, P., Banerjee, A., Szebehely, M., Armstrong, H., Daly, T., and Lafrance, S. (2009). ‘They Deserve Better’: The Long-term Care Experience in Canada and Scandinavia. Ottawa: Canadian Centre for Policy Alternatives.
Armstrong, P. and Laxer, K. (2013). “Demanding Labour: An Aging Health Care Labour Force.” Poster Presentation, OLTCA Applied Research Day.
Armstrong , P. and Silas, L. (2014). “Nurses Unions: Where Knowledge Meets Know-How.” In Marjorie McIntyre and Carol McDonald (Eds.), Realities of Canadian Nursing: Professionals, Practice and Power Issues. (pp.158-180). New York: Walters Kluwer/Lippincott Williams and Wilkins.
Armstrong, P. et al. (2002). Exposing Privatization: Women and Health Care Reform in Canada. Aurora: Garamond Press.
Aronson, J. and Neysmith, S. (1997). “The Retreat of the State and Long-term Provision: Implementations for Frail Elderly People, Unpaid Family Carers and Paid Home Care Workers.” Studies in Political Economy, 53(Summer), 37-66.
Banerjee, A., Daly, T., et al. (2008). “Out of Control: Violence Against Personal Support Workers in Long-term Care.” Toronto, York University.
B.C. Nurses’ Union. (2004). “Ensuring the Care We Need. Membership Polling for Bargaining 2004.”
Bourgeault, I. L. et al. (2010). Brain Gain, Drain and Waste: The Experiences of Internationally Educated Health Professionals in Canada. University of Ottawa.
Bracci, C. (2000). “Ties That Bind: Ontario’s Filial Responsibility Act.” Canadian Journal of Family Law, 17(2), 455-500.
Brotman, S. (1998). “The Incidence of Poverty Among Seniors in Canada: Exploring the Impact of Gender, Ethnicity and Race.” Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 17(2), 166-185.
Buchignani, N. and Armstrong-Esther, C. (1999). “Informal Care and Older Native Canadians”. Ageing and Society, 19(1), 3-32.
Campbell, L. D. and Martin-Matthews, A. (2000). “Caring Sons: Exploring Men’s Involvement in Filial Care.” Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 19 (1, Spring), 57-79.
Canada, Commission on the Future of Health Care in Canada. (2002). Building on Values: The Future of Health Care in Canada — Final Report (Romanow Report). Ottawa: Author.
Canada, Health and Welfare Canada. (1986). Achieving Health for All: A Framework for Health Promotion (Ottawa Charter). Ottawa: Author.
Canada, Minister of National Health and Welfare. (1974). A New Perspective on the Health of Canadians (Lalonde Report). Ottawa: Author.
Canadian Institute for Health Information. (2002). Canada’s Health Care Providers. Ottawa: CIHI.
Canadian Institute for Health Information. (2013). Canada’s Health Care Providers. Ottawa: CIHI.
Chubachi, N. (1999). “Geographies of Nisei Japanese Canadians and Their Attitudes Towards Elderly Long-term Care.” M.A. Queen’s University, Kingston, Ontario.
Clement, W. and Myles, J. (1994). Relations of Ruling: Class and Gender in Postindustrial Societies. Montreal: McGill-Queen’s University Press.
Coburn, J. (1987). “‘I See and Am Silent’. A Short History of Nursing in Ontario, 1850-1930.” In David Coburn, Carl D’Arcy, George Torrance and Peter New (Eds.), Health and Canadian Society, Second Edition. Markham: Fitzhenry and Whiteside.
Cohen, M. G. (2001). “Do Comparisons Between Hospital Support Workers and Hospitality Workers Make Sense?” Report prepared for the Hospital Employees Union (CUPE), Burnaby.
Cranswick, K. (1999). “Help Close at Hand: Relocating to Give or Receive Care”. Canadian Social Trends, 55 (Winter), 11-13.
Dabboussy, M. and Uppal, S. (2012). “Work Absences in 2011.” Perspectives on Labour and Income, 24(2). Statistics Canada Catalogue no. 75-001-XIE
Decima Research. (2002). National Profile of Family Caregivers in Canada 2002. Ottawa: Health Canada.
Denton, M. (1997). “The Linkages Between Informal and Formal Care for the Elderly.” Canadian Journal on Aging, 16(1).
Dhawan, S. (1998). “Caregiving Stress and Acculturation in East Indian Immigrants: Caring for Their Elders.” Ph.D, Queen’s University, Kingston, Ontario.
Dorazio-Migliore, M. (1998). “Eldercare in Context: Narrative, Gender, and Ethnicity.” Ph.D, University of British Columbia, 1999.
Duxbury, L. and Higgins, C. (2012). Revisiting Work-Life Issues in Canada: 2012 National Study on Balancing Work and Caregiving in Canada.
Duxbury, L., Higgins, C. and Shroeder, B. (2009). Balancing Paid Work and Caregiving Responsibilities: A Closer Look at Family Caregivers in Canada. Ottawa: Human Resources and Skills Development Canada.
Findorff, M. J. et al. (2004) “Risk Factors for Work Related Violence in a Health Care Organization.” Injury Prevention, 5 (October 10), 296-302.
Freidson, E. (1970). “Dominant Profession, Bureaucracy and Client Services.” In W.R. Rosengren and M. Lefton (Eds.), Organizations and Clients. Columbus, Ohio: Merrill.
Galarneau, D. (2004). “Health Care Professionals.” Perspectives on Labour and Income, 16(1, Spring), 16-29.
Gaskell, J. (1986). “Conceptions of Skill and the Work of Women: Some Historical and Political Issues.” In Roberta Hamilton and Michèle Barrett (Eds.), The Politics of Diversity. (pp. 361-384). Montreal: Book Center.
Gignac, M. A. M., Kelloway, E. K. and Gottlieb, B. H. (1996). “Impact of Caregiving on Employment: A Mediational Model of Work-family Conflict.” Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 15(4), 525-542.
Grant, K. et al. (Eds.) (2004). Caring For/Caring About: Women, Home Care and Unpaid Caregiving. Aurora: Garamond Press.
Grant, K et al. (Eds.) (2012). Thinking Women and Health Care Reform in Canada. Toronto: Canadian Scholars’ Press.
Guberman, N. (1999). Caregivers and Caregiving: New Trends and Their Implications for Policy. Ottawa: Health Canada.
Guberman, N. (2004). “Designing Home and Community Care for the Future: Who Needs Care?” In Karen Grant et al. (Eds.), Caring For/Caring About: Women, Home Care and Unpaid Caregiving. (pp. 75-90). Aurora: Garamond Press.
Hall, R., McKeown, L. and Roberts, K. (2001). Caring Canadians, Involved Canadians: Highlights from the 2000 National Survey of Giving, Volunteering and Participation. Ottawa: Ministry of Industry.
Institute of Work and Health. (2011). “Health-Care Rx: Reducing Work Absences Among Canadian Nurses.” At Work, 66.
Jansen, P. (1988). “The Changing Role of Nurses’ Unions.” In A. Baumgart and J. Larsen (Eds.), Canadian Nursing Faces the Future. Toronto: C.V. Mosby.
Johnson, T. (1972). Professions and Power. London: Macmillan.
Jones, F. (2000). “Youth Volunteering on the Rise.” Perspectives on Labour and Income, 12(1, Spring), 36-42.
Keefe, J. M. and Fancey, P. (1997). “Financial Compensation or Home Help Services: Examining Differences Among Program Recipients.” Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 16(2), 254-278.
Laxer K. (2013). “Counting Carers in Long-term Residential Care.” In Pat Armstrong and Susan Braedley (Eds.), Troubling Care: Critical Perspectives on Research and Practices. Toronto: Women’s Press.
Le Jeune, G., Belisle, A. and Messing, K. (2008). “The Data Gap in Canadian Women’s Occupational Health.” Policy and Practice in Health and Safety, 6(2), 51-81.
Lilly, M. B., Laporte, A. and Coyte, P. C. (2007). “Labour Market and Home Care’s Unpaid Caregivers: A Systematic Review of Labor Force Participation Rates, Predictors of Labor Market Withdrawl, and Hours of Work.” Milbank Quarterly, 85(4), 641-90.
Lilly, M. B., Laporte, A., and Coyte, P. C. (2010). “Do They Care Too Much to Work? The Influence of Caregiving Intensity on the Labour Force Participation of Unpaid Caregivers in Canada.” Journal of Health Economics, 29(6), 895-903.
Lindsay, C. (2008). Are Women Spending More Time on Unpaid Domestic Work Than Men in Canada? [Component of Statistics Canada Catalogue no. 89-630-X].
Luffman, J. (2003). “Volunteering on Company Time.” Perspectives on Labour and Income, 15(2, Summer), 34-40.
MacBride-King, J. L. (1999). Caring About Caregiving: The Eldercare Responsibilities of Canadian Workers and the Impact on Employers. Ottawa: The Conference Board of Canada.
Messing, K. (1998). One-eyed Science: Occupational Health and Women Workers. Philadelphia: Temple University Press.
Morgan, D. G., Stewart, N. J. et al. (2005). “Work Stress and Physical Assault of Nursing Aides in Rural Nursing Homes With and Without Dementia Special Care Units.” Journal of Psychiatric and Mental Health Nursing, 12, 347-358.
Morris, J. M. et al. (1999). “The Changing Nature of Home Care and Its Impact on Women’s Vulnerability to Poverty.” Ottawa; Status of Women Canada.
Mussallem, H. (1988). “The Changing Role of the Canadian Nurses’ Association in the Development of Nursing in Canada.” In J. Kerr and J. MacPhail (Eds.), Canadian Nursing Issues and Perspective. Toronto: McGraw-Hill Ryerson.
National Forum on Health. (1997). “Values Working Group Synthesis Report.” Canada Health Action: Building on the Legacy. Vol. II. [Synthesis Reports and Issues Papers]. Ottawa: Public Works and Government Services.
Poland, B. et al. (1998). “Wealth, Equity and Health Care: A Critique of a ‘Population Health’ Perspective on the Determinants of Health.” Social Science and Medicine, 46(7), 785-98.
Raphael, D. (2009). Social Determinants of Health. (2nd Ed.). Toronto: Canadian Scholar’s Press.
Raphael, D., Bryant, T. and Rioux, M. (2006). Staying Alive: Critical Perspectives on Health, Illness & Health Care. Toronto: Canadian Scholars’ Press.
Rosenberg, H. (1990). “The Home is the Workplace.” In Meg Luxton, Harriet Rosenberg and Sadef Arat-Kroc, Through the Kitchen Window. Toronto: Garamond Press.
Rosenthal, C. J. and Martin-Matthews, A. (1999). Families as Care-providers Versus Care-managers? Gender and Type of Care in a Sample of Employed Canadians. Sedap Research Paper No. 4, McMaster University.
Shamian, J. and Villeneuve, M. (2004). “Meeting the Growing Demand for Nurses.” Health Policy Research Bulletin Issue, 8(May), 23-27.
Sinha, M. (2012). “Portrait of Caregivers.” Spotlight on Canadians: Results from the General Social Survey No. 1.
Snell, J. G. (1990). “Filial Responsibility Laws in Canada: An Historical Study.” Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 9(3), 268-277.
Statistics Canada. (1999). Labour Force Update, 4(2). [Statistics Canada Cat. No. 71-005-XPB].
Statistics Canada. (2000). Women in Canada 2000: A Gender-based Statistical Report. [Statistics Canada Cat. No. 89-503 XPE]. Ottawa: Minister of Industry.
Statistics Canada. (2012a). Women in Canada at a Glance: Statistical Profiles. Ottawa: Statistics Canada.
Statistics Canada. (2012b). “Study: Employer Support of Volunteering, 2010.” The Daily.
Stone, D. (1988). Policy, Paradox and Political Reason. New York: Harper Collins.
Turcotte, M. (2013). “Family Caregiving: What Are the Consequences?” Insights on Canadian Society. Ottawa: Statistics Canada.
Vezina, M. and Crompton, S. (2012). “Volunteering in Canada.” Canadian Social Trends, 93, 37-55.
Vogel, L. (2003). The Gender Workplace Health Gap. Brussels: European Trade Union Technical Bureau for Health and Safety.
Vosko, L. F., MacDonald, M. and Campbell, I. (Eds.). (2009). Gender and the Contours of Precarious Employment. New York: Routledge.
Wilkinson, R. and Pickett, K. (2010). The Spirit Level: Why Equality is Better for Everyone. London: Penguin Books.
Wilkinson, R. G. (1992). “Income Distribution and Life Expectancy.” British Medical Journal, 304, 165-68.
Willis, E. (1983). Medical Dominance. Sydney: George Allen and Unwin.
Witz, A. (1992). Professions and Patriarchy. New York: Routledge.
Yantzi, N. M., Rosenberg, M. W., and McKeever, P. (2007). “Getting Out of the House: The Challenges Mothers Face When Their Children Have Long-term Care Needs.” Health & Social Care in the Community, 15(1), 45-55.
Yassi, A. and Hancock, T., (2005). “Patient Safety, Worker Safety: Building a Culture of Safety to Improve Healthcare Worker and Patient Well-being.” Healthcare Quarterly, 8(32), 32-38.
Zukewich, N. (2003). “Unpaid Informal Caregiving.” Canadian Social Trends, 70 (Autumn), 14-18.
